Navigating the Path Forward for Dementia in Canada: The Landmark Study Report #1
Canada needs bold action to head off an impending dementia care crisis. This report from the Alzheimer Society of Canada says actions to reduce risk have potential to change the future of dementia in Canada — if governments act now.
Report formats
On September 6, 2022, the Alzheimer Society of Canada released this report about dementia in Canada. It's the first of three reports we will being released about the Landmark Study from 2022 to 2025. Download the report PDF or scroll down to read more.
September 2022
The first of a series of three reports on dementia prevalence and costs in Canada, this volume covers the projections of people living with dementia in Canada from 2020 to 2050. It also recommends actions to reduce the risk of dementia that could potentially change the future of dementia in Canada.

Foreword by Dr. Brian Goldman
Dementia is arguably the greatest health challenge of Canada’s aging society. What makes it all the more daunting is not knowing the scale of the challenge and its impact on Canadians.
The Landmark Study seeks to fill the data gap with a microsimulation study whose intent is to project the number of people who will develop dementia in Canada by the year 2050, and assess the impact of factors such as age, sex, ethnicity, health status and geography.
The numbers generated by this report are staggering.
By the year 2050, more than 1.7 million Canadians are expected to be living with dementia, with an average of 685 individuals being diagnosed each day.
All told, that translates into an estimated 6.3 million Canadians diagnosed, living with and eventually dying of dementia over the next 30 years. Women with dementia will continue to outnumber men diagnosed with this condition. It’s up to researchers to find out why.
The impact of dementia on Canada’s health-care system will be huge.
In Canada, family doctors and nurse practitioners are primarily responsible for diagnosing and providing health care for persons with dementia. If projections are correct, the demand for primary care services will grow even as fewer medical students are choosing family medicine as a career.
Within the offices and clinics of primary care providers, patients with dementia will require a disproportionate share of their time. The provinces and territories need to incentivize family doctors and nurse practitioners to provide customized care to these highly complex patients.
It is imperative that we make our best efforts to delay the onset of dementia, if not prevent it outright.
As the Landmark Study reveals, there are many things Canadians can do to improve their health and reduce the impact of dementia. These include being physically and socially active; following a healthy diet; challenging one’s brain by engaging in games, reading, learning new languages, hobbies and skills; managing stress; quitting smoking; limiting alcohol consumption; and preventing head injuries by wearing a helmet. Canadians also need to partner with their health-care provider to manage blood pressure and diabetes.
The Landmark Study shows us how impactful these measures can be in aggregate. Delaying the onset of dementia by 1 year would avoid nearly 500,000 cases of dementia over the next 30 years in Canada. Delaying the onset by 10 years would effectively avoid more than 4 million cases.
Dementia has a disproportionate impact on loved ones. I know this personally because I helped care for my mother when she had dementia. Now, just eight years following her death, I have once again found myself providing essential care for a close family member.
In the years ahead, I will not be exceptional. The Landmark Study reveals that by the year 2050, more than 1 million Canadians will serve as care partners to people with dementia. The care they provide will be equivalent to more than 1.4 billion hours per year or 690,000 full-time jobs.
Care partners, as the Landmark Study calls them, are often taken for granted by our society.
To enable them to carry out the tasks expected of them, we need to support them financially and emotionally, and give them the training they need to do the work properly. Caregiving is stressful, which means we need to provide them with respite care as needed.
The Landmark Study gives us a roadmap to follow over the next 30 years. There is much that we can and should do to begin the journey.
Executive summary
Introduction
In Canada, over 600,000 people from British Columbia to Nunavut to Newfoundland and Labrador are living with dementia.
Those who live with Alzheimer’s dementia (that is, dementia caused by Alzheimer's disease), with vascular dementia, and with other forms of dementia (including young-onset dementia) and their family and friends are all deeply affected by the cognitive decline, memory loss, changes in mood and behaviour, and loss of functional abilities that can occur.
There is some hopeful news on preventing or delaying the onset of dementia.
However, population aging in Canada means we will continue to see ongoing increases in the number of people affected by dementia. While we have made progress in the last decade to better address this brain condition, much more work needs to be done.
With this report, we aim to achieve the following:
- Clarify the path forward. The first objective of this report is to update public knowledge of dementia numbers across Canada and how we expect these counts to change over the next 30 years.
- Improve knowledge. Dementia is a complex condition with many established risk factors. This report aims to break down the complexity and highlight key areas for risk reduction.
- Advocate for individuals, families, care partners, and service providers. Most individuals who develop dementia do not face the challenge alone. Family, friends and neighbours often help support people living with dementia. The people contributing both formal and informal care need support and resources.
- Create action. Inspire individuals, researchers, health-care providers, funding agencies, and the various levels of governments to support and work toward programs and policies that promote better brain health for all.
- Push for change. There is a need for action: more dollars for research, changes to our care systems, recognizing and reducing discrimination, stigma and stereotypes, and implementing equitable solutions for the challenges that come with the onset of dementia.
About this report and series of reports
This report is the first of a series of three releases that will share our results. In this first report, we cover the following areas:
- Chapter 1: The Current Direction of Dementia in Canada
- Chapter 2: The Need for Care—It’s Not an Individual Journey
- Chapter 3: The Power of Prevention and Delaying Dementia Onset
- Chapter 4: Differences in Dementia Rates Across Regions of Canada
- Chapter 5: Finding the Best Path Forward
In the second report, we will provide additional focus on the people who will experience
dementia in Canada over the next three decades:
- Differences between sexes
- Expected population shifts in the ethnicity of people living with dementia
- Young-onset dementia
In the final report, we will use the simulation model to examine the economic impact of dementia in Canada.
Chapter overviews and key insights
Chapter 1: The current direction of dementia in Canada
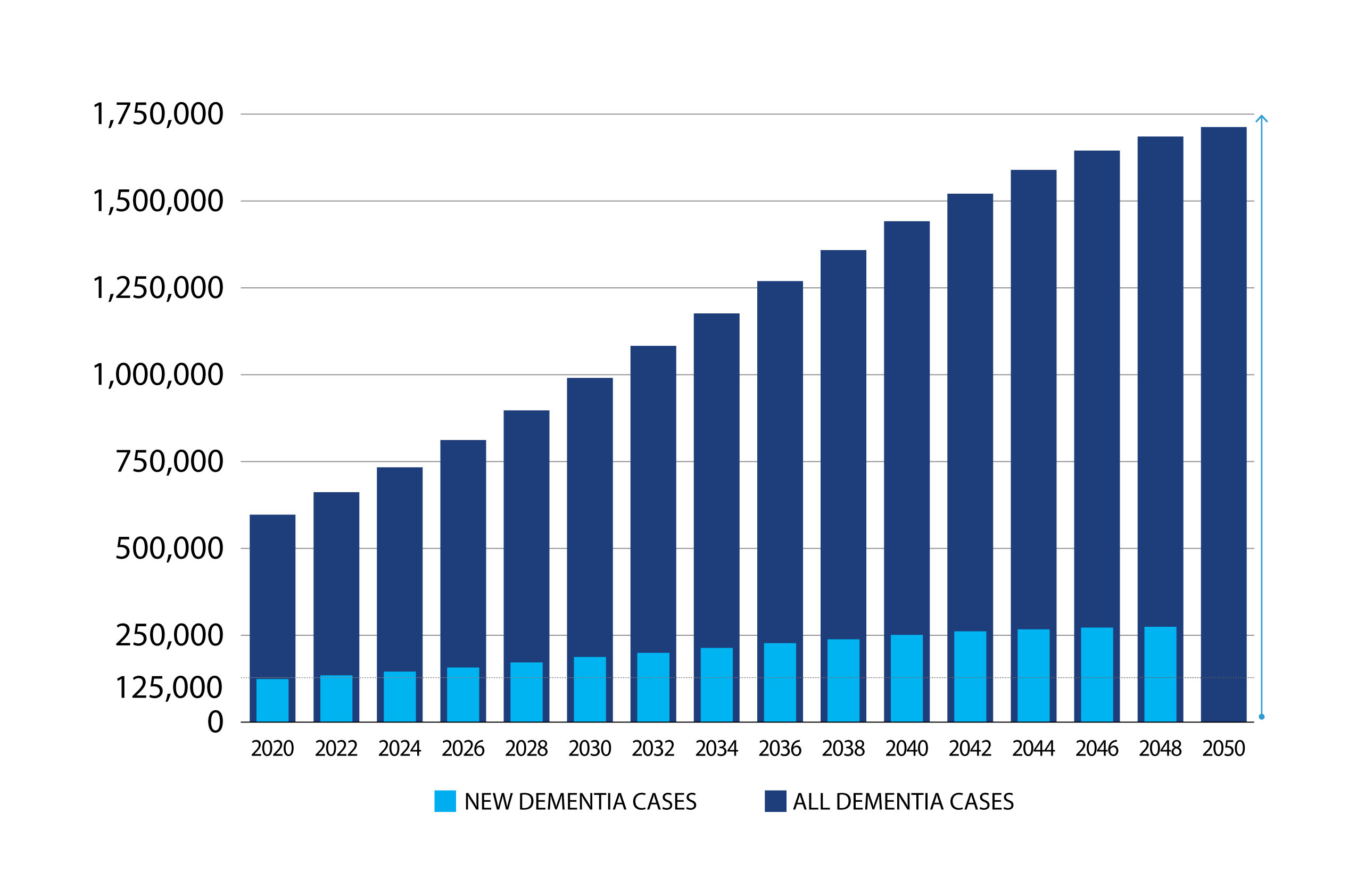
In 2020, it was estimated that there were 597,000 individuals living with dementia in Canada. By 2030, we can expect this number will reach close to 1 million.
In terms of new cases per year—what epidemiologists call annual incidence—in 2020 there were 124,000 new cases of dementia diagnosed (10,333 per month; 348 per day; 15 every hour). By 2030, the annual incidence will rise to 187,000 new cases a year (15,583 per month; 512 per day; 21 every hour).
If we look further into the future, using the latest demographic trends from Statistics Canada combined with our Landmark Study model, we can also predict that the challenges that come with dementia in Canada will further intensify in the 2030s and 2040s.
In terms of annual incidence, by the 2040s it is expected that over 250,000 individuals will develop dementia each year (20,833 per month; 685 per day; 29 every hour).
By 2050, the number of people living with dementia will almost triple the 2020 level, and over 1.7 million Canadians will be living with dementia.
Chapter 2: The need for care—it’s not an individual journey
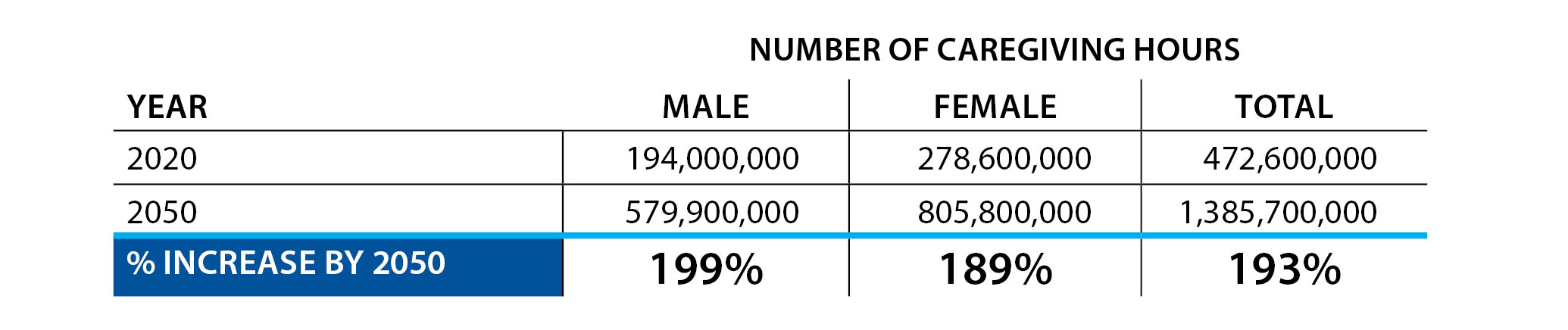
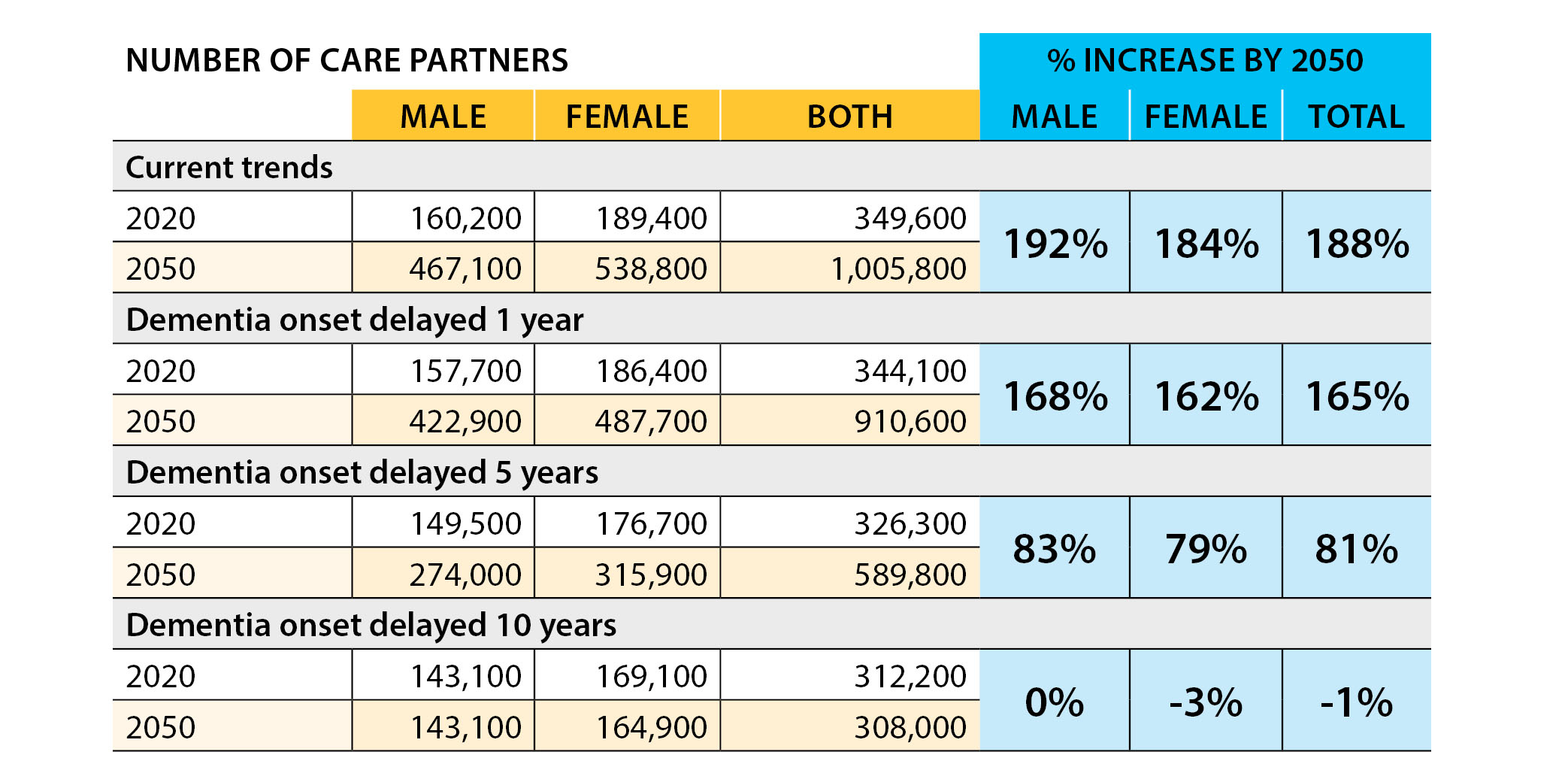
Our study found that in 2020 there were 350,000 care partners for people with dementia. With an average of 26 hours of care per week, together this amounts to 470 million hours of care in a year.
This number of hours is equivalent to 235,000 full-time jobs (40 hours per week with 2 weeks vacation)—a tremendous contribution of time and resources by care partners for those living with dementia in Canada.
If you translate these hours into dollar figures, even at a federal minimum wage of $15.55 per hour, the care provided by family and friends is greater than $7.3 billion dollars.
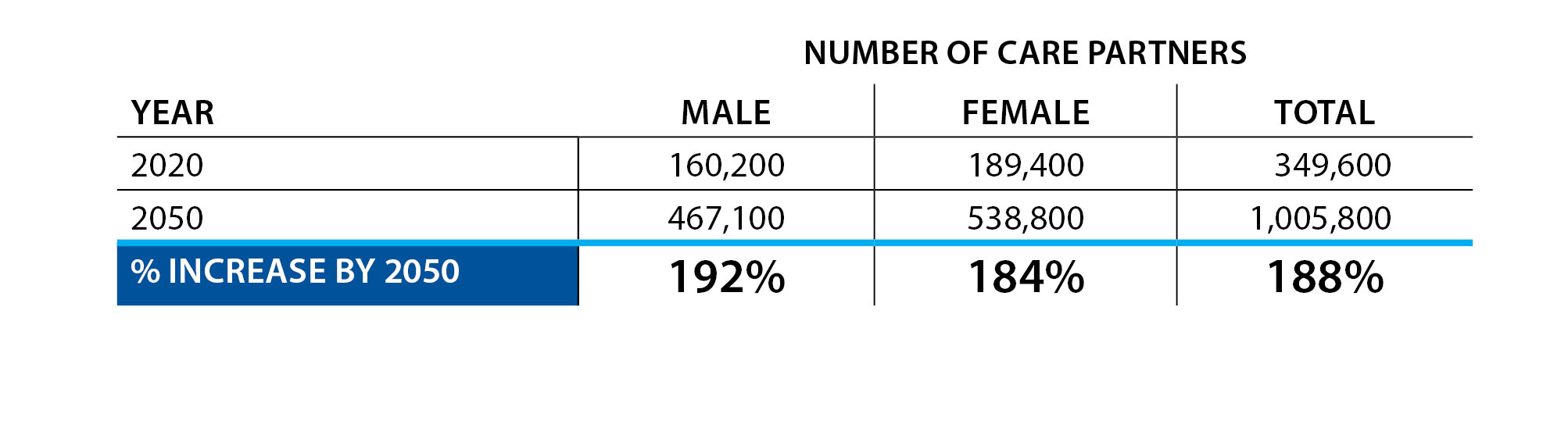
Our projections suggest that if not much changes in the current trends, by 2050 the number of care partners for people living with dementia will increase to over 1 million in Canada. This would be almost tripling (188% increase) the number of care partners over the 30-year period.
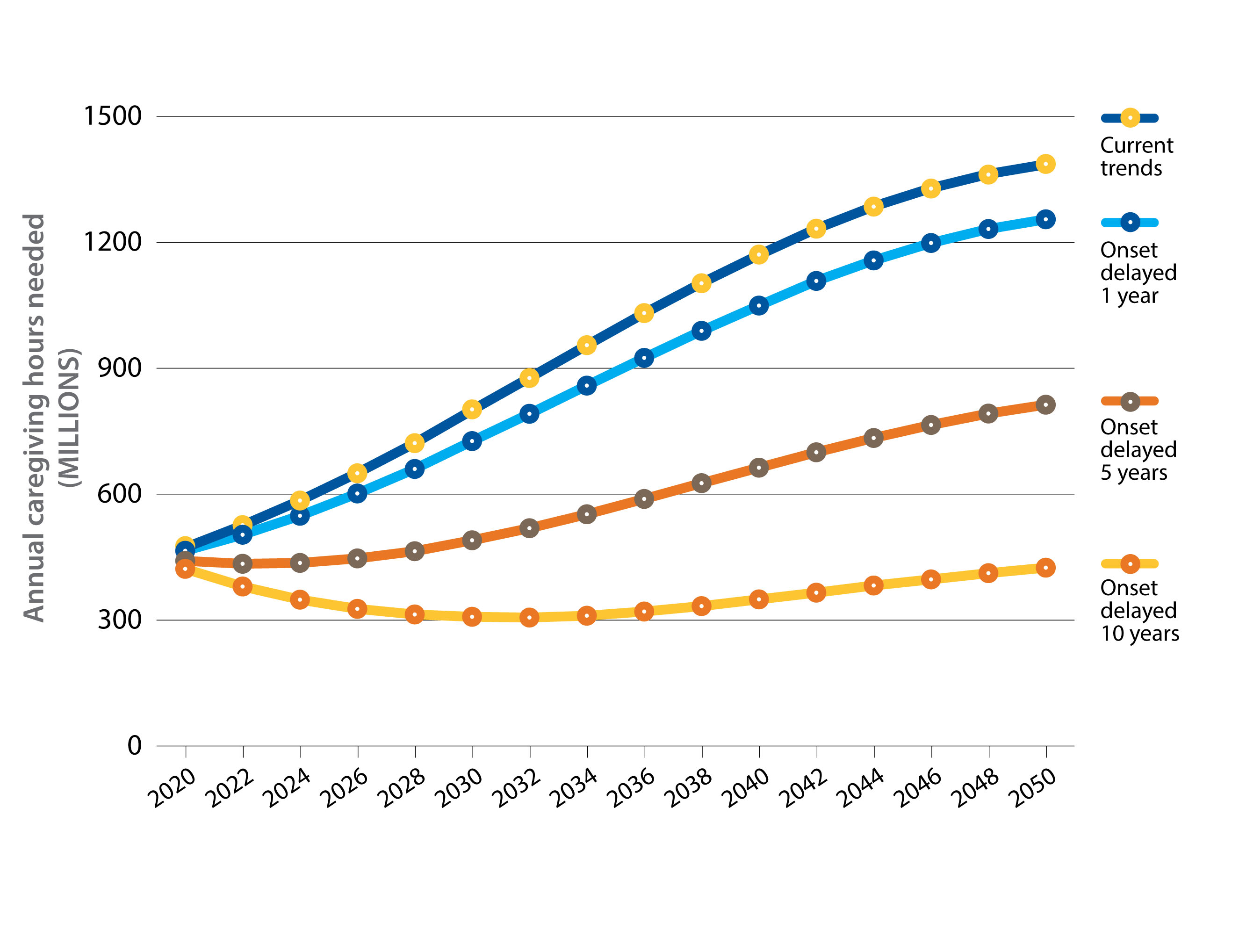
Given the large number of people living with dementia, and the level of care required, the number of hours provided by family could reach almost 1.4 billion hours annually by 2050. This is equivalent to over 690,000 full-time jobs.
Chapter 3: The power of dementia risk reduction
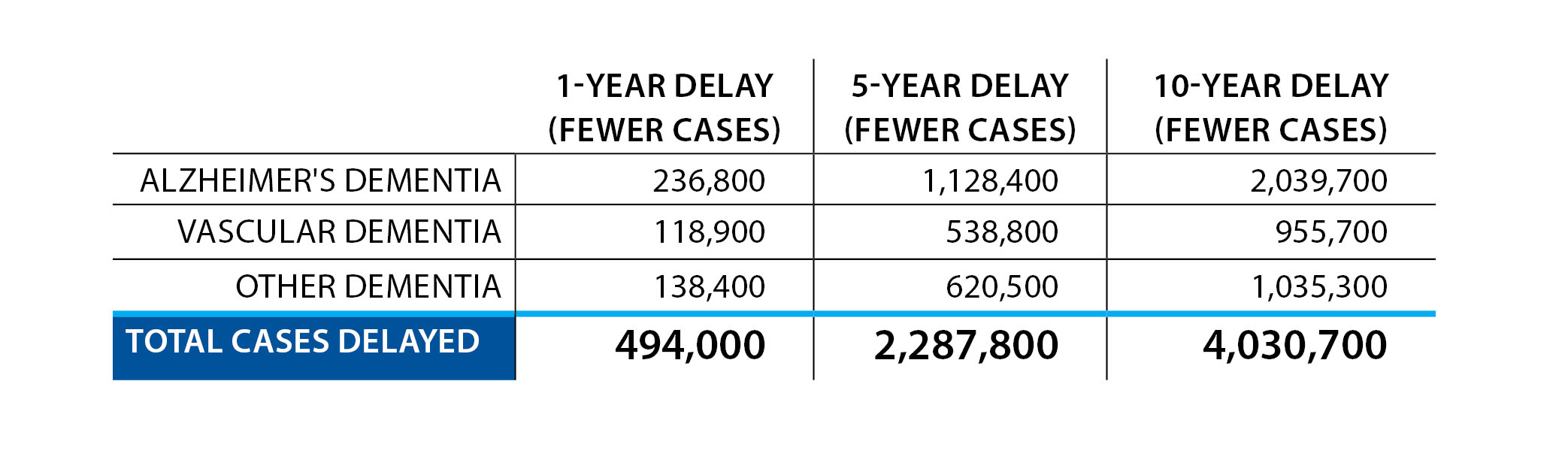
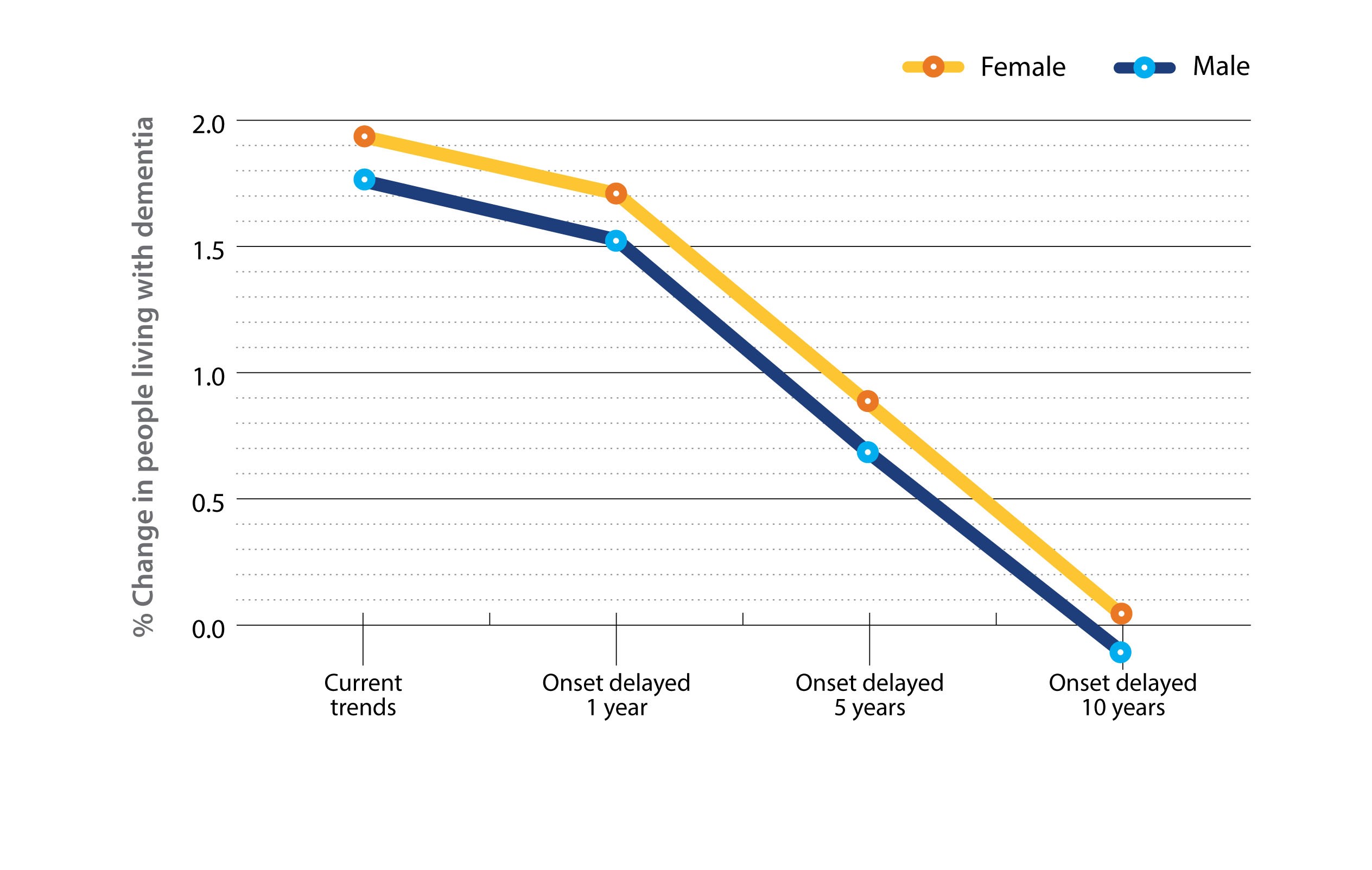
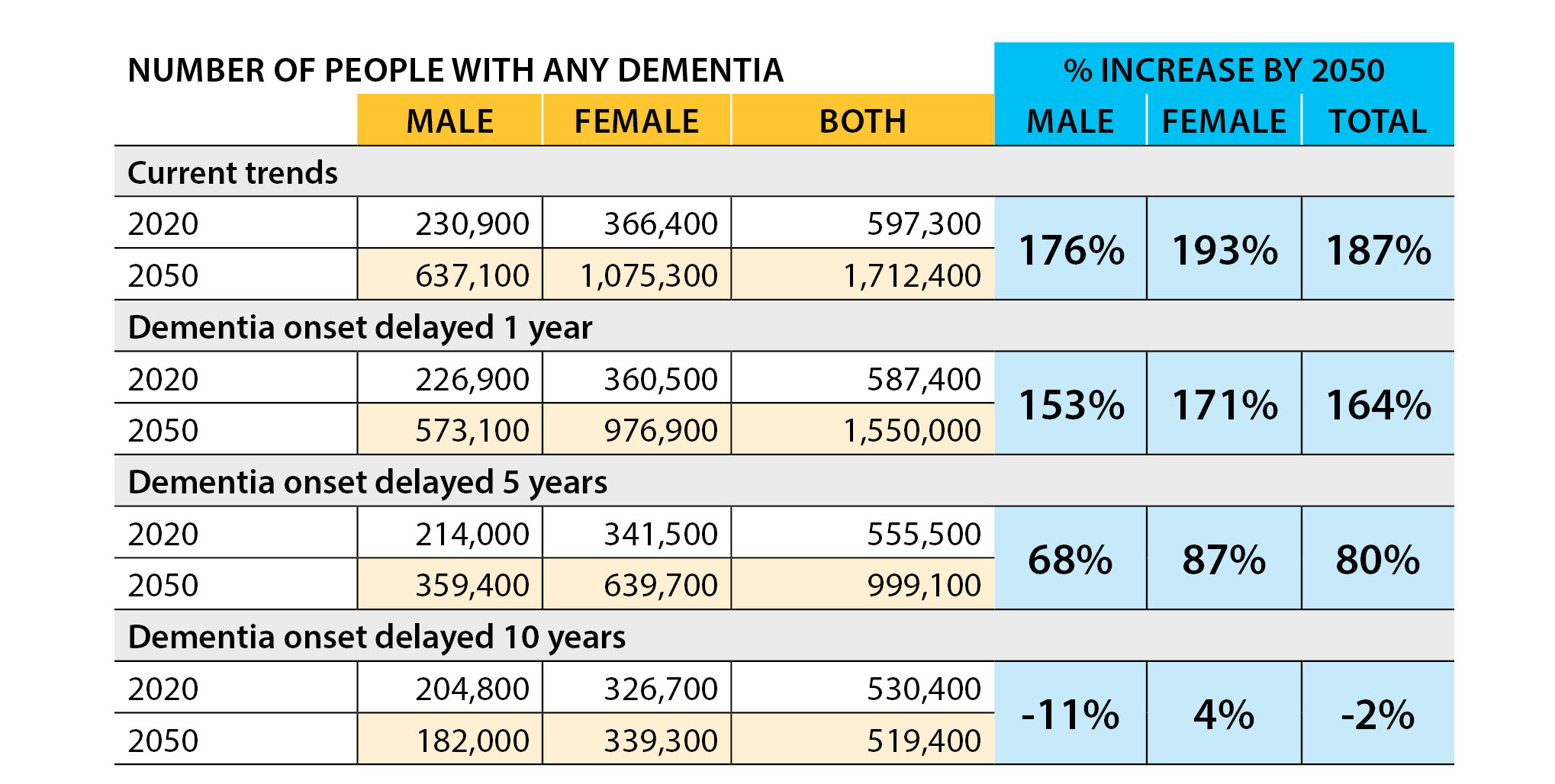
The Landmark Study developed three hypothetical scenarios where the onset of dementia in Canadians was delayed by 1, 5 or 10 years. The goal of these scenarios is to demonstrate what the effect would be on the Canadian population if we were able to improve prevention efforts for dementia and delay its onset across our population.
All three hypothetical scenarios demonstrate the power of
prevention. Even a delay of 1 year could result in almost 500,000 fewer new cases by 2050; this would make a huge difference in national dementia rates across the next three decades. If the onset of dementia could be delayed by 10 years, over 4 million new cases of dementia could be avoided by 2050.
Delaying the onset of dementia could also have an enormous impact on caregiving for people living with dementia in Canada. A 10-year delay could reduce the number of caregiving hours needed by almost 1 billion hours per year.
Chapter 4: Differences in dementia rates across regions of Canada
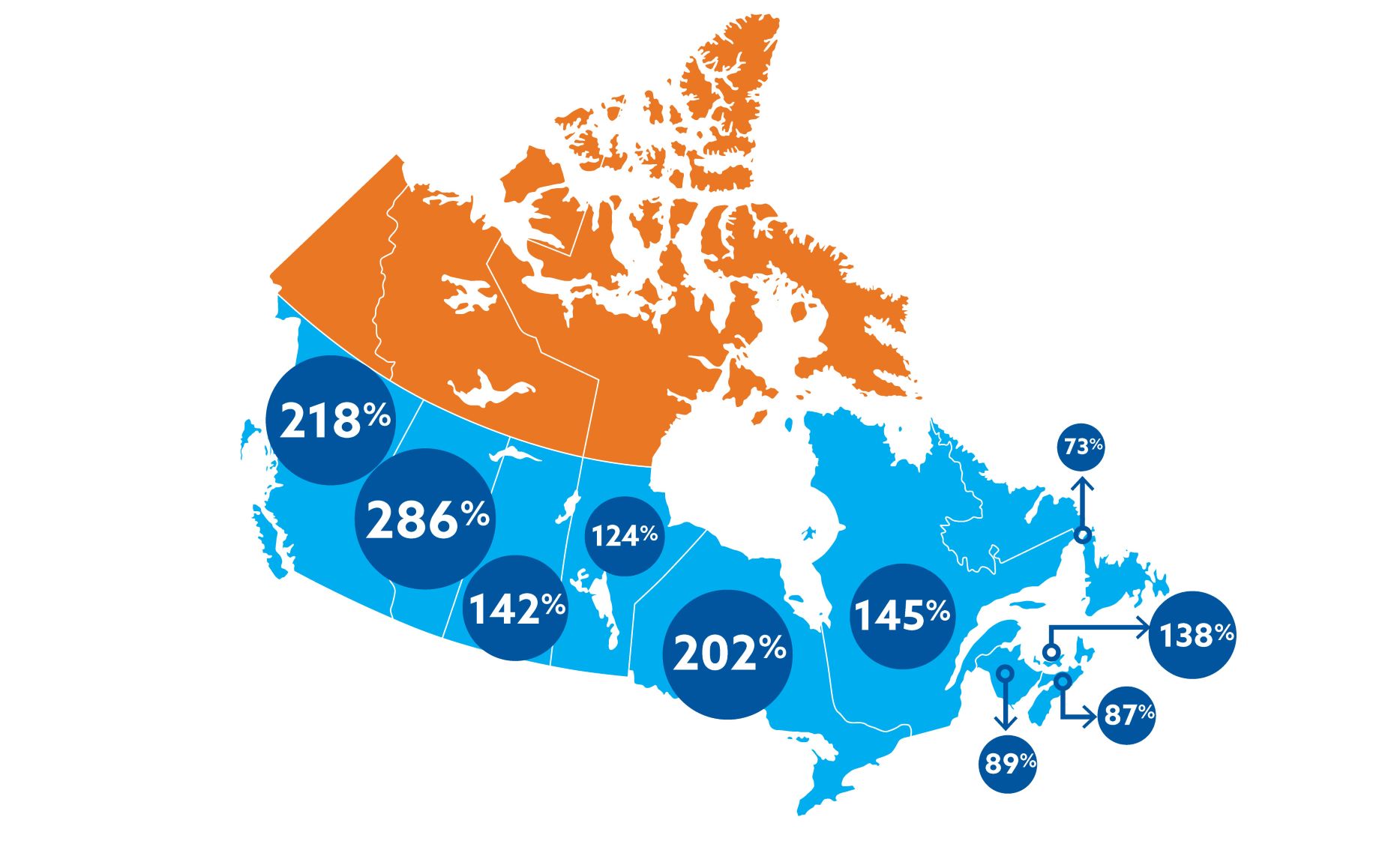
All regions of Canada are expected to see an increase in the number of people with dementia if current trends continue. However, the growth in dementia cases will not be uniform across the country.
Dementia will affect the provinces differently over the next 30 years. Differences in age distributions, migration patterns, and the prevalence of risk factors combine to produce specific challenges, needs, and overall numbers of people living with dementia for each province.
Unfortunately, insufficient data was available to study the Yukon, the Northwest Territories or Nunavut.
Chapter 5: Finding the best path forward
Dementia will continue to be a growing issue in Canada, with the number of people living with some form of dementia projected to triple over the next 30 years.
If current trends continue, all regions of the country will see a dramatic increase in the number of people with dementia and the demands placed on care partners.
While a cure or an effective treatment for dementia has not yet been discovered, a wide range of actions can be taken to optimize the dementia journey for people in Canada.
The final chapter of the report highlights some of the actions that can lead to positive outcomes for people living with dementia and their care partners.
All people in Canada have a role to play in this challenge. As a result, recommendations in the report have been organized to address these perspectives: What do Alzheimer Societies do? What can health-care systems do? What can the federal, provincial/territorial and municipal levels of government do? What can researchers do? What can individual Canadians do?
Across all of these lists, it is important that this work is done collaboratively with people living with dementia and their care partners.
Where the data for this study came from
The Landmark Study is a microsimulation study we undertook to project the number of people who will develop dementia over the next 30 years in Canada. The study uses the socio-economic statistical analysis platform from the Canadian Centre for Economic Analysis (CANCEA) to make these projections.
A microsimulation model is similar to the way simulation video games like SimCity work. Rather than setting up a city in a game and looking at how interactions and events occur over simulated time, our model uses publicly available data from Statistics Canada to create “agents” that are used as a statistical representation of persons living in Canada. Each agent is associated with several demographic characteristics, including age, sex, ethnicity and health status, which match those of the Canadian population.
The model can simulate the agents and their interactions over time as the agents age and pass through various health states, such as dementia diagnosis, risk factor exposure, hospitalization and death. This allows the model to provide estimates and forecasts of the rates of dementia in Canada over time and the care needs for people with dementia.
This model also lets us ask what might happen in Canada if the age at which dementia begins is delayed by 1, 5 or 10 years. This helps us understand the potential impact of effective dementia risk reduction efforts on a national level.
More details about the methods of the Landmark Study model are found in the Appendix.
Chapter 1: The current direction of dementia in Canada
Introduction
In 2010, the Alzheimer Society of Canada produced the Rising Tide report, which brought attention to the dementia epidemic that was beginning to rise in the Canadian population.
At that time, just under half a million people in Canada lived with Alzheimer’s dementia or other dementias, and many more family members, friends, and neighbours were being affected through their “informal” caregiving roles.
The Rising Tide report called for a national plan to prepare for and mitigate the challenge of dementia in Canadian society. In 2019, the federal government produced A Dementia Strategy for Canada. This strategy, along with its annual updates, can be found on the Government of Canada website.
The federal dementia strategy has been a great step toward better managing dementia in Canada.
But the findings of our new Landmark Study, some of which are detailed in this report, demonstrate that we must take further action now if we are to meet the challenge of the surge in dementia that has already begun in Canada.
The data suggests that:
- Every day in 2022, an average of over 350 people in Canada are diagnosed with dementia (from the Landmark Study findings).
- For every person in Canada who has dementia, a family member or friend will spend an average of 26 hours a week caring for them.
- Billions of dollars are spent on health-care costs and out-of-pocket individual and care partner expenses in supporting people living with dementia in Canada.
Additional gaps show that:
- We have an incomplete understanding of risk and protective factors for dementia development and the progression of dementia—more needs to be done. This is especially important as there is no known cure for dementia.
- The home care and long-term care systems in Canada are already under strain and facing multiple crises, with urgent need to remodel dementia care.
- While many care partners report the positive aspects of providing care, care partners of all ages and types (spouses, children, friends, neighbours) too frequently experience challenges, including financial hardship, burnout, depression and isolation.
Based on projections from the Landmark Study, the impact of these challenges will grow—not only in the number of people experiencing them, but also in their severity.
Canada’s health-care and long-term care systems are already struggling, and the expected rise in the number of Canadians affected by dementia will exacerbate these difficulties. COVID-19 highlighted some of the pre-existing challenges in these systems, which will only increase if we continue to do things as we have done in the past (e.g., underfunding health care).
Although we have a better sense of risk factors for dementia than we did 10 years ago, the social will, social action, and social support needed to act on this knowledge are still lacking. We expect that this report will make a further case to encourage change.
A note on word choice: “Alzheimer's disease” and “Alzheimer's dementia”
The term “Alzheimer’s disease” refers to an illness that causes changes to brain structure years before any problems with thinking, memory, mood, communication or behaviour emerge.
The term “Alzheimer’s dementia” refers to a later stage of that same disease; during this stage, problems with thinking, memory, mood, behaviour and/or communication are evident.
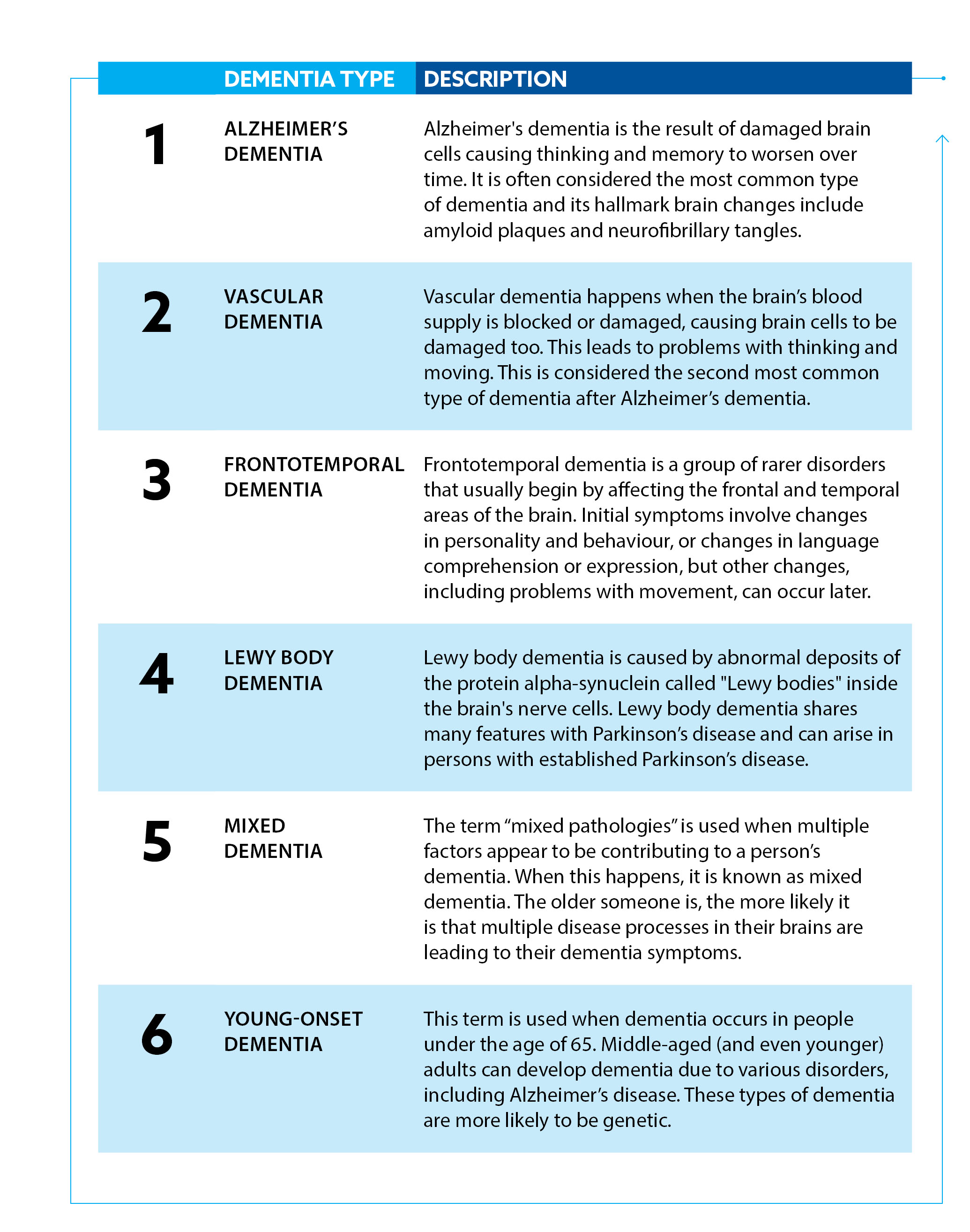
There are many different subtypes of dementia
Dementia is a word that describes a set of symptoms caused by specific disruptions to healthy brain functioning that reduce a person’s ability to perform everyday activities. These symptoms can include (but are not limited to) memory loss, difficulties with attention, problem solving and language; changes in mood and behaviour; and issues with vision, balance, and movement.
There are several different subtypes of dementia. Some of the more commonly seen types are outlined in Box 1. We now know that many people with dementia often have features of more than one type.
Risk factors for dementia
While age is the primary factor associated with the onset of dementia, dementia is not a normal part of aging.
Many people experience some cognitive changes as they get older, but only a small percentage develop dementia that progresses from mild to severe over a number of years.
Nonetheless, Canada’s population is quickly aging—in just 5 years (2016–2021), the percentage of Canadians over the age of 65 rose from 16.9% to 19.0% (Statistics Canada, 2022a). We can expect a corresponding rise in the number of older adults experiencing some form of dementia.
We still have an incomplete understanding of the mechanisms that lead to dementia, but researchers have pinpointed several risk factors that increase the chance that someone will develop dementia.
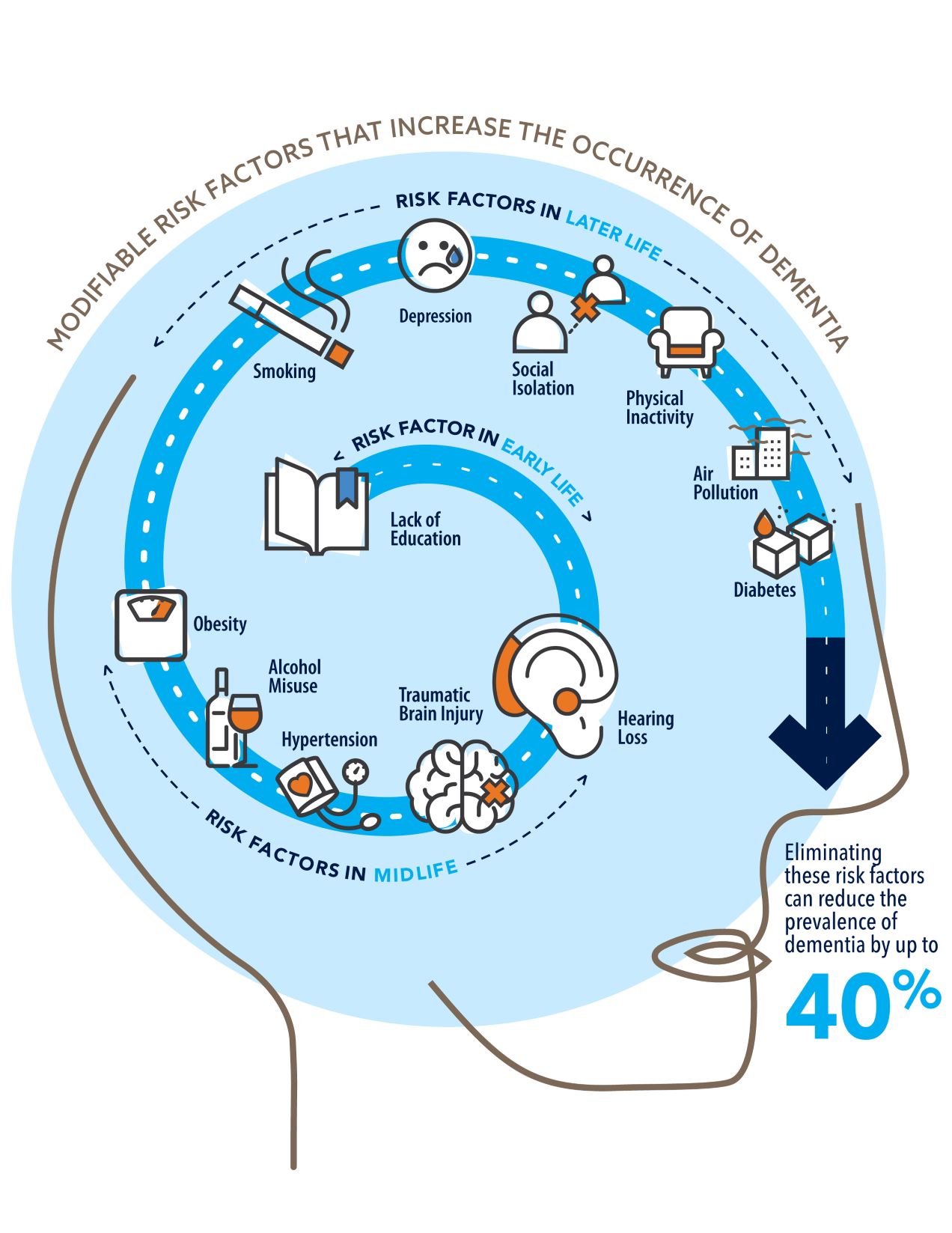
Importantly, some factors can be changed or modified to delay or reduce the risk of developing dementia. These factors affect people differently across their life course (i.e., from birth to middle age to older age). Select examples are listed in Box 2.
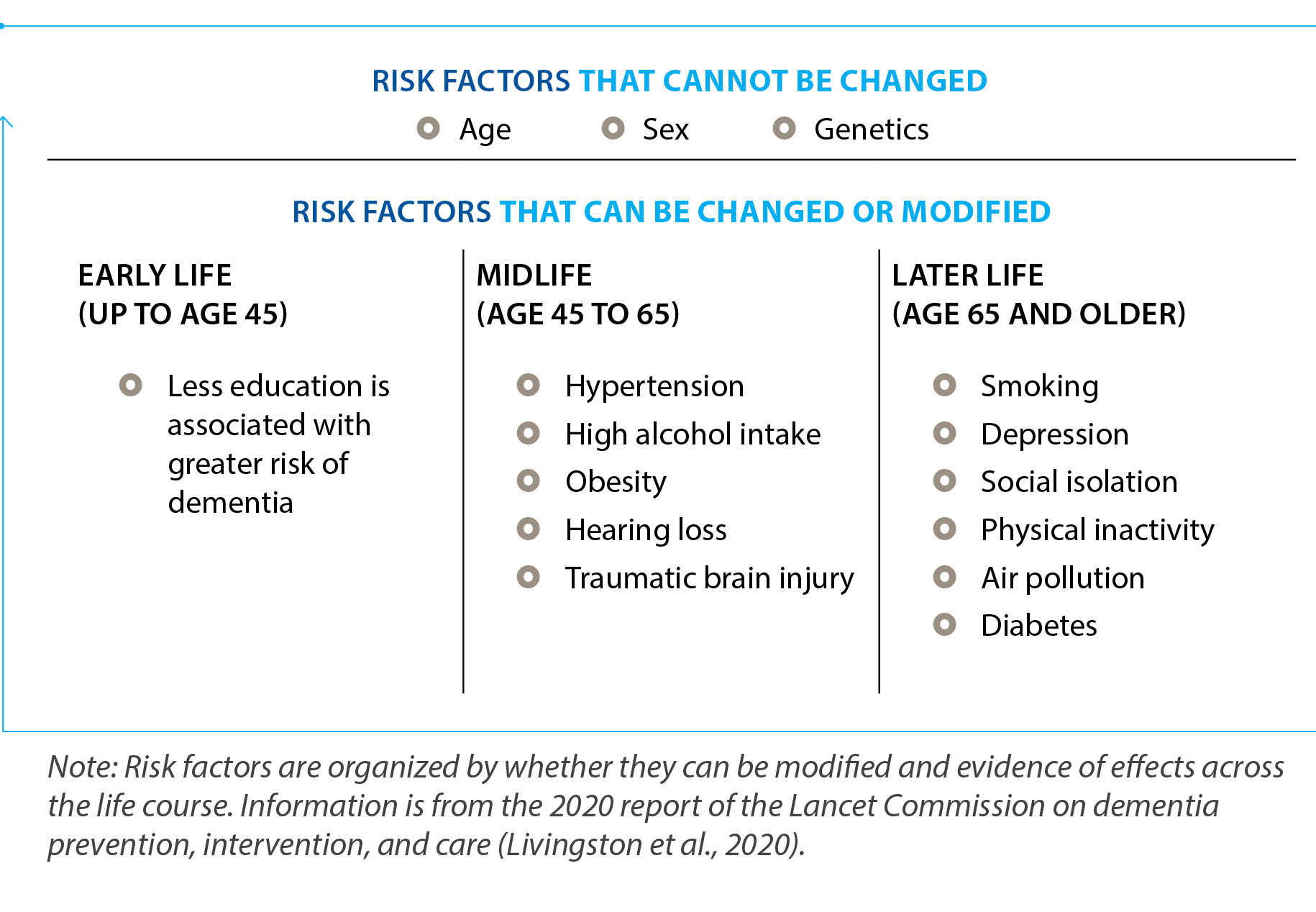
Of the list of risk factors for dementia, age remains the most important. While it is not considered a direct cause of dementia, it is closely associated with risk of dementia onset.
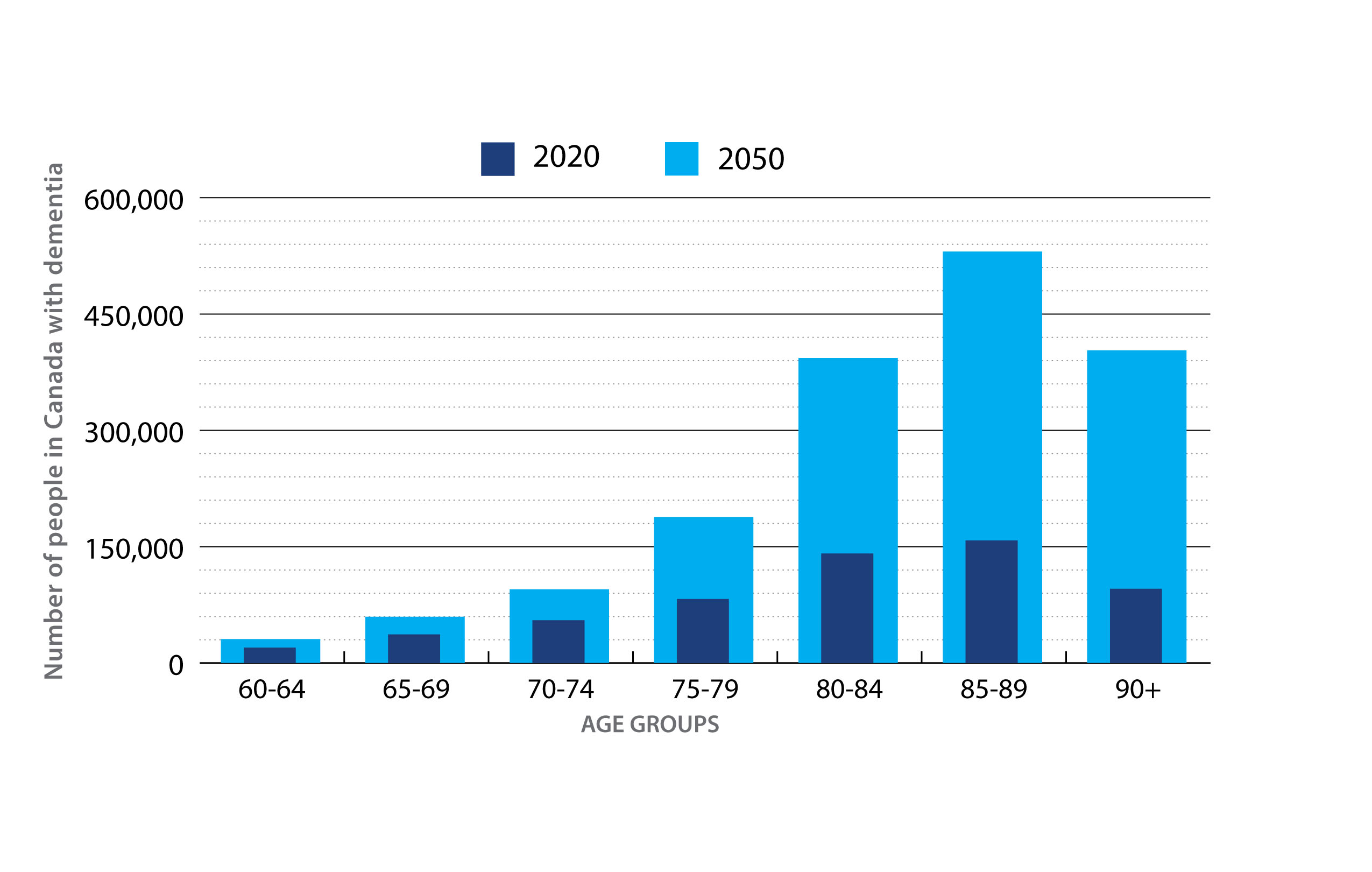
For example, most (but not all) people who develop dementia are over the age of 65. After the age of 65, the risk of dementia approximately doubles every five years. After the age of 85, nearly one in every four Canadians has been diagnosed with dementia.
As expected, with the size of our older population increasing quickly, population aging plays a strong role in what the Landmark Study projects for the expected number of people living with dementia in Canada over the next 30 years.
A million Canadians with dementia by 2030
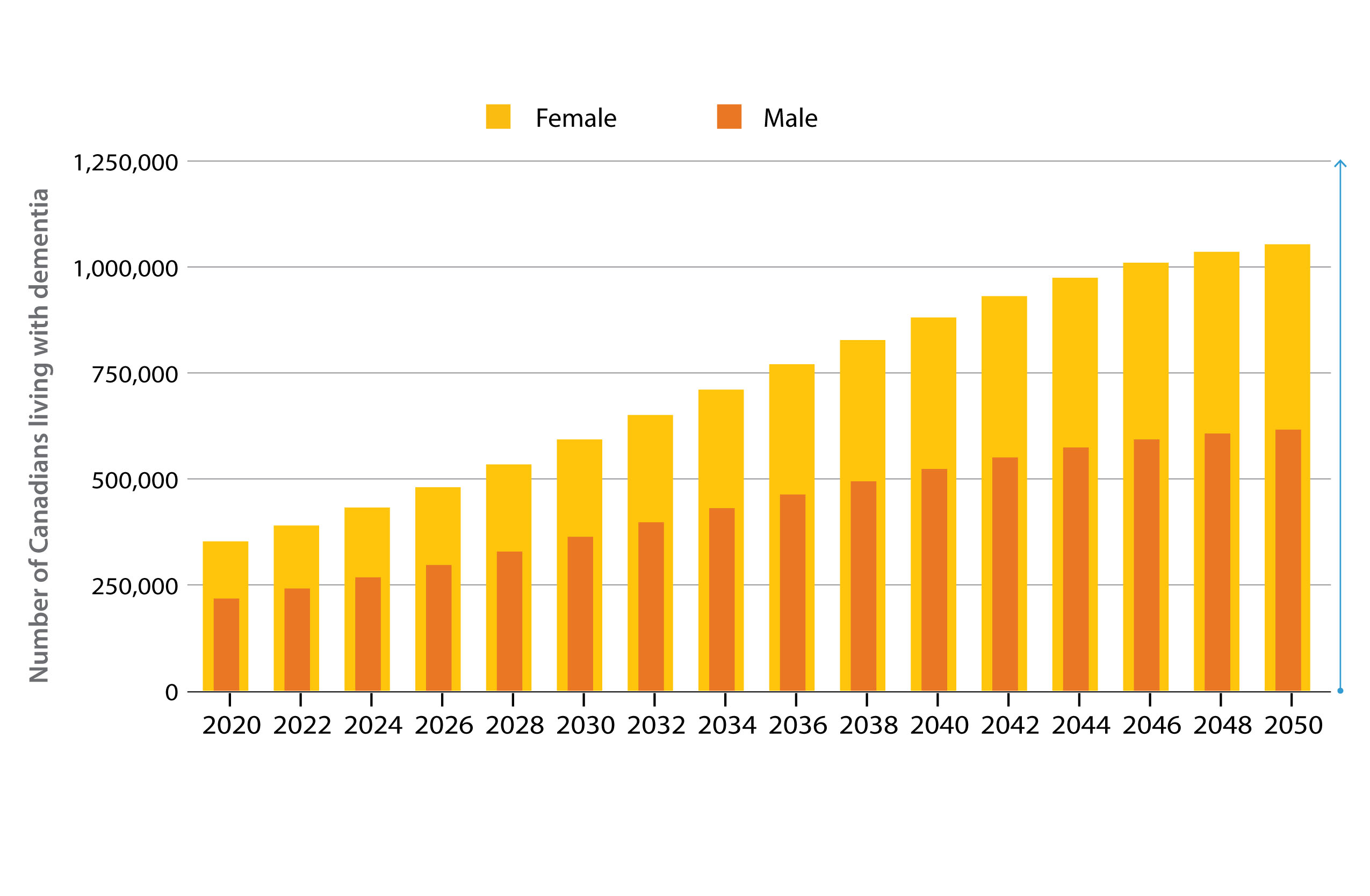
In 2020, it was estimated that there were 597,300 individuals living with dementia in Canada. By 2030, we can expect this number will reach close to 1 million (Figure 1).
In terms of new cases per year—what epidemiologists call annual incidence—in 2020 there were 124,000 new cases of dementia diagnosed (10,333 per month; 348 per day; 15 every hour). By 2030, the annual incidence will rise to 187,000 new cases a year (15,583 per month; 512 per day; 21 every hour).
These expected changes mean that, compared with 2020 numbers, by 2030 we can expect a 51% increase in the number of new cases per year and an overall increase of 65% in the number of Canadians living with dementia (597,300 —> 990,600).
These short-term estimates for higher numbers of individuals living with dementia in 2030 indicate a pressing need to increase levels of health and social care—by our health and long-term care systems, home care, and family/friend care partners.
Can our current systems handle this increase? How can we best meet this challenge across these levels of care?
We hope that the Landmark Study will inspire both immediate and long-term actions to meet the needs of the growing number of people in Canada living with dementia.
Increasing age is the primary risk factor for dementia
The increasing number of people in Canada living with dementia is primarily a function of an aging population. Dementia will steadily become more common as the “baby boomer” cohort (the large group of people born between 1946 and 1965) ages into their eighties and nineties.
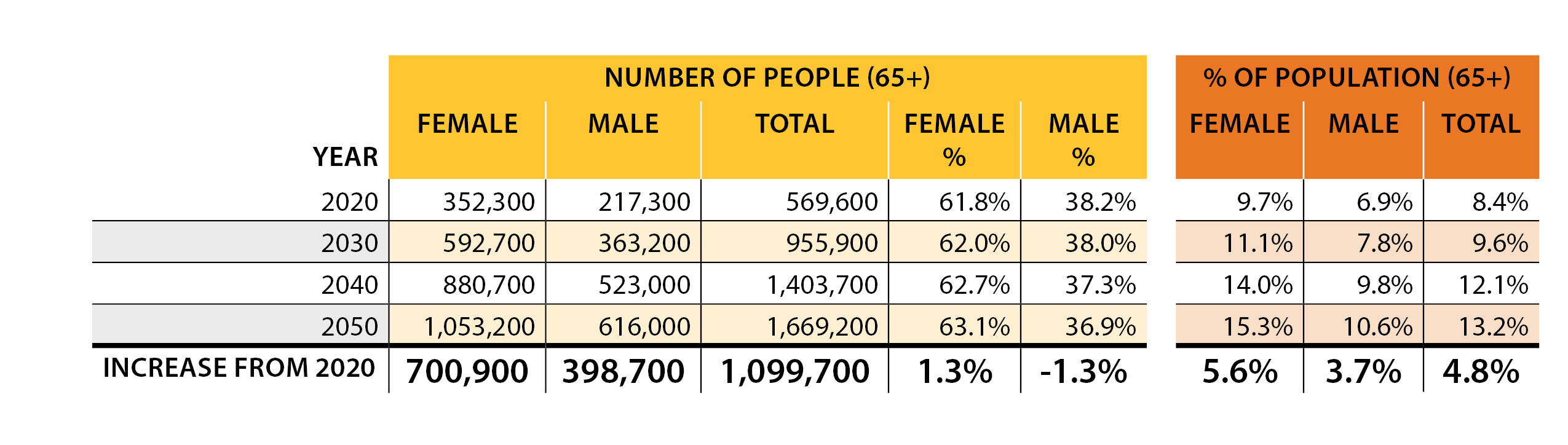
In 2020, 8.4% of Canadians over 65 had some form of dementia. By 2050, when all the surviving baby boomer generation is 85 or older, the percentage of Canadians over 65 living with dementia is expected to increase to 13.2% (Table 2).
The largest estimated increases in dementia are in the older age groups, with the number of people over 85 with dementia expected to increase almost 30% faster than the overall number of cases in the population.
According to the latest Statistics Canada reports (2022a), the number of Canadians over the age of 85 is expected to triple by 2046, which directly relates to some of the projections made by this study. Figure 2 shows a comparison of dementia numbers for 2020 with expected numbers for 2050, according to different age groups.
20,000+ Canadians will be diagnosed every month in the 2040s
If we look further into the future, using the latest demographic trends from Statistics Canada combined with our Landmark Study model, we can also predict that the challenges that come with dementia in Canada will further intensify in the 2030s and 2040s.
In terms of annual incidence, by the 2040s it is expected that over 250,000 individuals will develop dementia each year (20,833 per month; 685 per day; 29 every hour).
By 2050, the number of people living with dementia will almost triple the 2020 level, and over 1.7 million Canadians will be living with dementia (Figure 1).
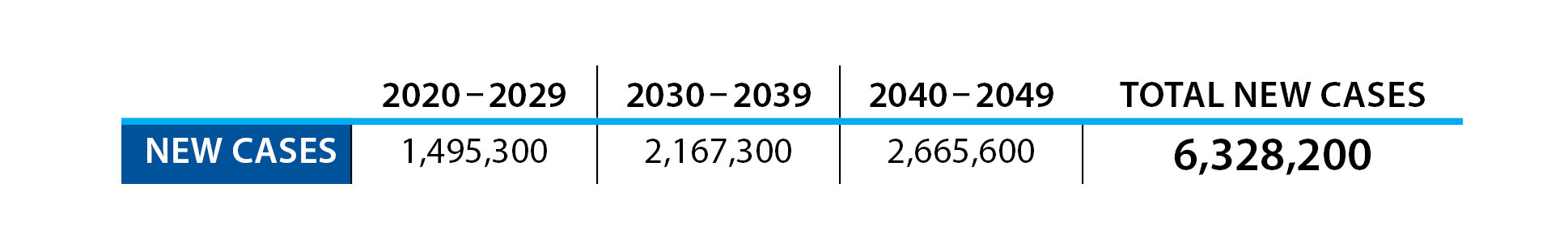
While about 1.6% of the Canadian population in 2020 had dementia, this number is expected to increase to 3.6% by 2050. Over this 30-year period, over 6.3 million individuals would develop dementia (Table 1).
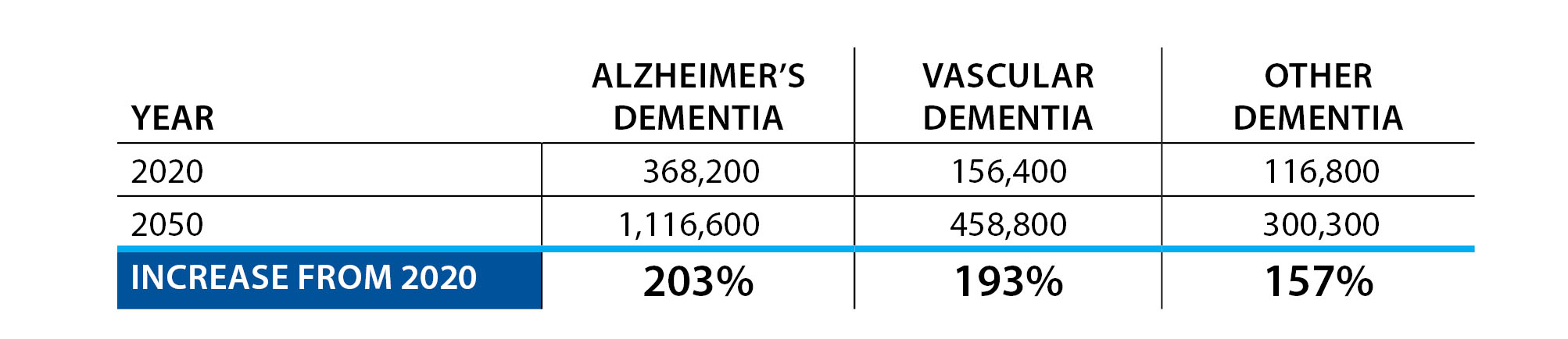
Alzheimer's dementia will remain the most common dementia
Alzheimer’s dementia will continue to be the dominant type of dementia in Canada in the coming decades, with over 1.1 million people affected by 2050. Projections of people living with vascular dementia have been estimated to be 460,000 in 2050, while 300,000 people are forecast to live with other forms of dementia by 2050 (Table 3).
We know that multiple diseases or conditions can affect the brain at the same time, resulting in what is called “mixed dementia.” Many scientists think mixed pathologies are truly the most common cause of dementia.
Often, an older adult’s brain might have the neurofibrillary tangles and amyloid plaques typical of Alzheimer’s dementia, but their brain may also show evidence of blood vessel damage, stiff and clogged arteries, changes to the white matter, cell loss, and accumulation of various other abnormal proteins. These “mixed pathologies” would be associated with both Alzheimer’s dementia and vascular dementia.
Determining the type of dementia a person might have by looking at physical changes in the brain is complex. This is especially true in the oldest groups of people; for them, many types of symptoms and injuries to brain structures have had time to accumulate.
Researchers are working on this problem by using ever-improving imaging technologies to examine the brains of people living with dementia, and by studying the brains of people that have been donated for scientific research after they have died.
With these approaches, among others, researchers will continue to grow our understanding of how a brain can become damaged—and how such damage might relate to the symptoms and signs of dementia.
More females than males are living with dementia
The number of females experiencing dementia is projected to continue to be significantly greater than the number of males (Figure 3). In 2020, an estimated 61.8% of persons living with dementia (352,000) in Canada were female. This gap between the sexes is projected to grow slightly to 63.1% in 2050.
Canada isn’t alone in this trend. When we look at dementia rates from around the world, women experience dementia more often than men by a considerable margin.
Women tend to live longer than men and increased age leads to an increased risk of dementia, but other factors are also likely contributing. These include biological factors such as sex differences in hormones; brain structure; health conditions causing inflammation; genetics; and frailty, which also tends to be higher in women than in men (Andrew & Tierney, 2018).
Further, this divide in dementia risk between the sexes may be driven by other factors: sex differences in cognitive abilities on the standard clinical tests used to diagnose dementia; gendered social roles that influence how clinicians judge losses of abilities; and different opportunities in education and occupation throughout the life course.
These sex and gender differences are further complicated when these factors interact and change as people get older. Much more attention to sex and gender differences in dementia is needed if we are to fully understand dementia and improve our ability to address it for all Canadians.
As the number of Canadians living with dementia increases, it will become of growing importance to address other population diversity—socio-economic status, race, ethnicity, language and disability. Further to this point on diversity, dementia research and the current available services are also lacking when it comes to many minority groups in Canada.
Chapter 2: The need for care—it's not an individual journey
Introduction
In Canada, most people living with dementia reside at home. In 2015 and 2016, 69% of seniors with dementia under the age of 80, and 58% of those over 80, lived in the community and outside of the long-term care systems (Canadian Institute for Health Information [CIHI], 2018a).
Most older adults in Canada want to maintain their independence and remain in their communities for as long as possible. But people living with advancing dementia often cannot manage their lives on their own.
In addition to the care provided by health and social care professionals (including the Alzheimer Societies), most people with dementia living at home will rely on the care and support of care partners.
These family members, friends and other volunteers who support the person living with dementia are commonly referred to as “informal caregivers.” This term is used because informal caregivers are not paid while providing this support.
Due to the progressive nature of most dementias, people with dementia who live at home will eventually need increasing levels of medical and social support, which may ultimately present challenges to their family and friends who act as care partners. Canadian statistics (CIHI, 2018b) have shown that for people living with dementia:
- 1 in 4 require a lot of help for activities of daily living
- (e.g., eating, dressing, personal hygiene)
- 1 in 4 exhibit various behavioural changes (e.g., anger, delusions, getting lost,
- restlessness, hallucinations, paranoia)
- 1 in 4 have symptoms of depression
- 1 in 4 were admitted to hospital at least once in the last three months
- 1 in 5 have been to an emergency room in the last three months
Who are care partners?
Care partners are family members, neighbours or friends who provide ongoing care to another person in need of support.
Most care partners for persons living with dementia are adult children. Of those providing dementia care in the home, 58% are children and 32% are spouses, while the remaining 10% include other family, friends or community members (CIHI, 2018b).
Statistics also show that women do the majority of the unpaid caregiving for people living with dementia (Statistics Canada, 2022b).
The role of care partners for people with dementia
Care partners for people with dementia provide an average of 26 hours of caregiving per week compared to 17 hours per week for older adults with other health issues (CIHI, 2018b).
The number of care hours is related to the severity of the dementia, caregiver characteristics, and changes in mood, personality and behaviour. These factors are also related to medical care costs and costs to society as a whole (Angeles et al., 2021).
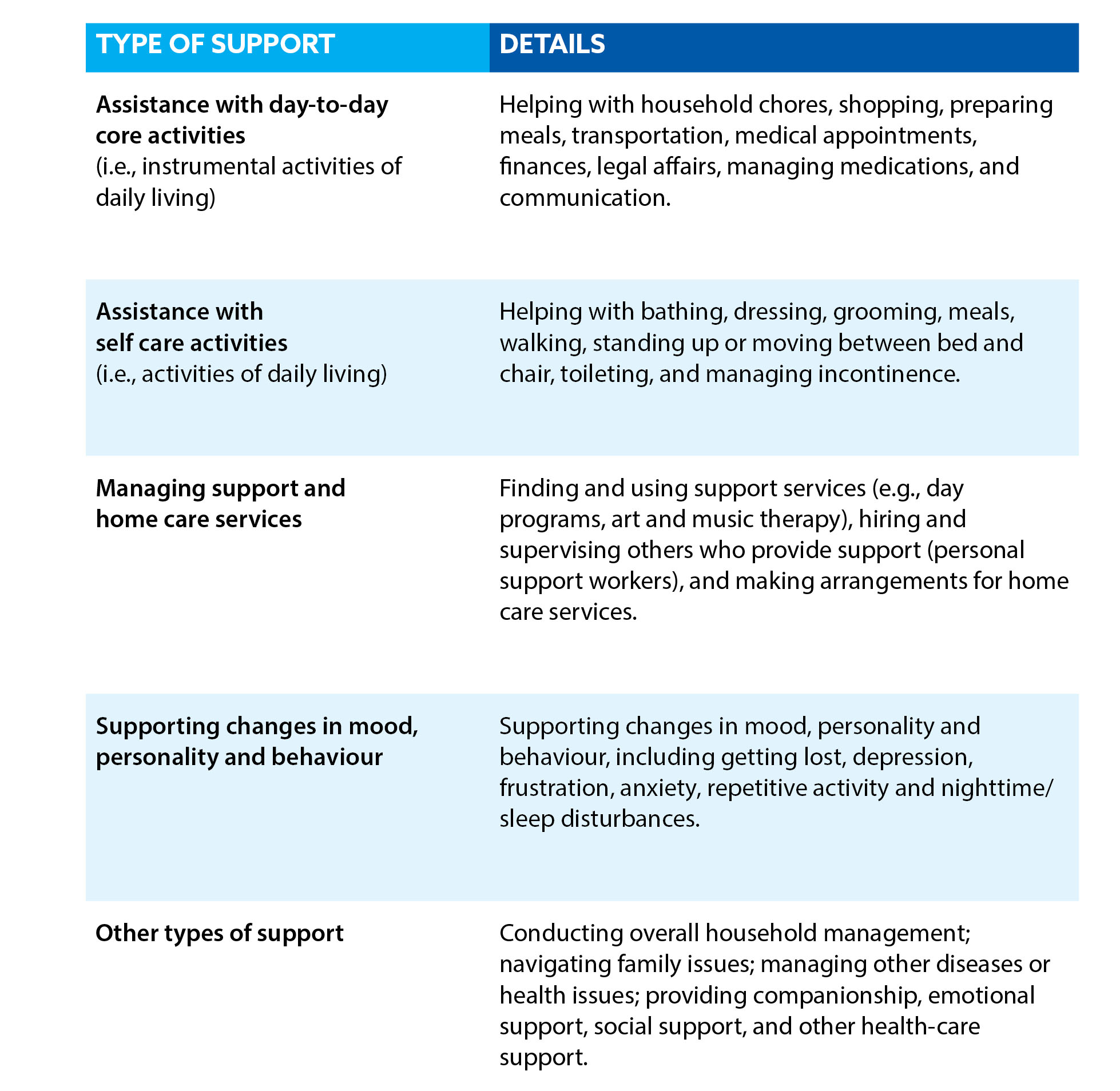
Areas of care that are commonly done by care partners can include:
- assistance with everyday activities (like household chores, meals and personal hygiene)
- support for medical care (such as arranging, coordinating and attending appointments;
- dispensing medications)
- supporting changes in mood, personality and behaviour that can occur for some
- people living with dementia
- providing psychological support, companionship, and advocacy in general
Further details for these types of supports can be found in Table 4.
Every care partner comes to their role with different resources, skills and needs. And the role of the care partner changes across the different stages of dementia (Huang et al., 2015). Changes occur in various ways:
- types of activities of support
- alignment of knowledge and skills with the activities and challenges of care
- volume of care and support provided
- amount of pressure, stress, and tension
Care partners who are family members or friends, many of them women in the middle stages of their lives, may step away from their jobs, lose out on career transitions, and miss out on time with their children and spouses to care for the person living with dementia.
Middle-aged Canadians who find themselves caring for an aging parent with dementia while still raising their own children are commonly described as the “Sandwich Generation”—a whole generation caring for both the young and the old.
Having the responsibility to care for both your children and your parents can lead to care partners feeling overwhelmed, stressed, and at a higher risk for burnout. Perhaps a better term for this group might be “Squeezed Generation,” as those with aging parents and young children must cope with the heavy pressure of trying to manage everyone’s needs, often contributing to their own health problems and burnout.
Care partner health and stress
While many care partners find their experiences rewarding, it is also important to recognize that the caregiving role can have a negative impact on the health and quality of life of the care partner.
Studies have shown that caring for a person with dementia can be more stressful than caring for a person with a physical disability (Ory et al., 1999). Care partners often become secondary patients due to the risks to both physical and emotional health that can come with providing hours of care for a family member or friend with dementia (Richardson, 2013; Zhu et al., 2014).
Data from the Canadian Institute for Health Information (2018b) reports that:
- 45% of care partners providing care to people living with dementia exhibit symptoms of distress. This is almost twice the rate compared to care partners of older adults with health conditions other than dementia (26%).
- 21% of care partners feel unable to continue their caring activities due to stress. The factors that are associated with care partner stress vary across individuals as well as across the progression of dementia (Bergvall et al., 2011; Pinquart & Sorensen, 2003). These factors can include:
- the number of hours of care provided
- the severity of personality, mood or behaviour changes of the care recipient
- the health status of the care provider and their external circumstances or stressors
- the level of dependence for completing functional activities of the care recipient
- the severity of cognitive impairment of the care recipient
Looking ahead with the Landmark Study, the increased number of people living with dementia will lead to a demand for an increased number of dementia care partners—this will add additional stress to the health-care system as many care partners are challenged to maintain their own health as well as that of the person they support.
Informal caregiving equals 235,000 unpaid full-time jobs
Our study found that in 2020 there were 350,000 care partners for people with dementia. With an average of 26 hours of care per week, together this amounts to 470 million hours of care in a year.
This number of hours is equivalent to 235,000 full-time jobs (40 hours per week with 2 weeks vacation)—a tremendous contribution of time and resources by care partners for people living with dementia in Canada.
If you translate these hours into dollar figures, even at a federal minimum wage of $15.55 per hour, the care provided by family and friends is worth greater than $7.3 billion dollars.
Of these care partners, approximately 54% were women. There was considerable variation in age groups:
- 12% were over 65
- 44% were 45–65
- 14% were 35–45
- 30% were under 35
Many working-age adults are providing care to persons living with dementia (307,000 under the age of 65 in 2020). With an average number of 26 hours per week spent caregiving, this role clearly affects a care partner’s ability to fully participate in the workforce and represents a large economic impact in Canada.
Over 1 million care partners for people living with dementia by 2050
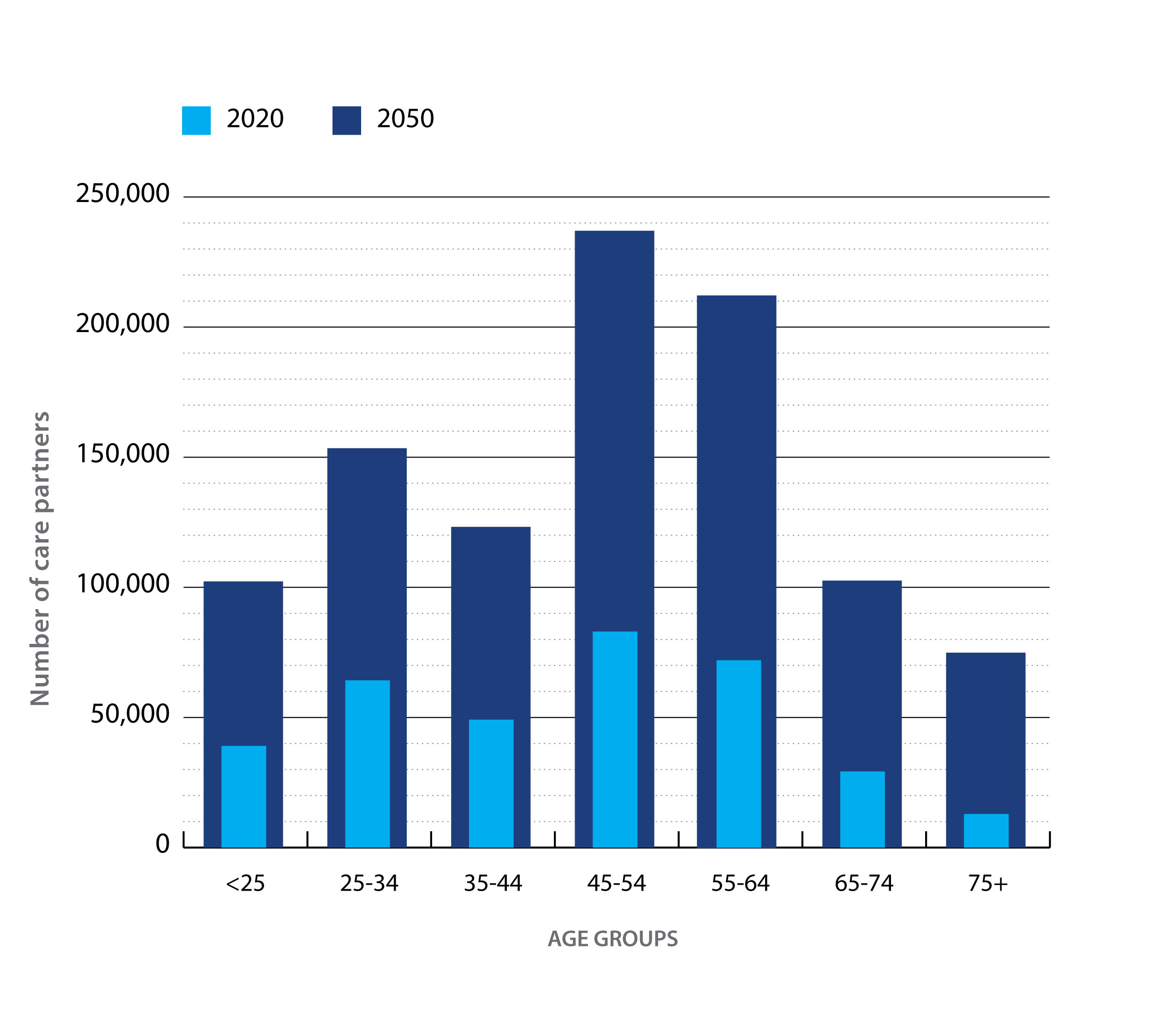
Our projections suggest that if not much changes in the current trends, by 2050 the number of care partners for people living with dementia will increase to over 1 million in Canada. This would be almost tripling (188% increase) the number of care partners over the 30-year period. (For more details, refer to Table 5.)
In the next 30 years, we expect a large increase in the number of middle-aged people (age 45–65) caring for people living with dementia. In 2020, the estimated number of care partners age 45 to 65 was 155,000. By 2050, this number is expected to almost triple to 449,000, an increase of 190% (Figure 4).
This large increase in the need for middle-aged care partners will have a direct impact on the workforce in Canada and on the Canadian economy. Both the health and careers of many care partners across Canada will be affected by dementia if the current trends prevail.
In addition to the growing impact on middle-aged Canadians, there is also an expected increase in older age groups where partners are providing care to their spouses while managing their own health challenges as they get older. This can lead to increased stress and exacerbation of the care partner’s own health issues (Statistics Canada, 2020).
A growing number of care partners are also younger than 35. For them, dementia caregiving may coincide and compete with completing secondary or post-secondary education, launching a career, and starting a family.
Unpaid caregiving impact equal to 690,000 full-time jobs in 2050
Given the projected increases in the number of people living with dementia, and the level of care required, the number of hours provided by family and friends could reach almost 1.4 billion hours annually by 2050 (Table 6). This is equivalent to over 690,000 full-time jobs.
Since we depend so much in Canada on these care partners, we must optimize available resources and supports so they can best manage the role they have taken on. This support is the responsibility of everyone, from health-care providers to Alzheimer Societies and all levels of government.
Chapter 3: The power of dementia risk reduction
Introduction
Dementia is often described as a public health challenge about which nothing can be done because it is due to the aging of the population—but this is false.
Research has demonstrated that there are actions that can be taken that may help reduce the risk of developing dementia. While some risk factors like age, sex at birth and genetics cannot be changed, others can. These are known as modifiable risk factors.
Non-modifiable risk factors for dementia are factors that may increase your chance of developing dementia and that cannot be changed. Examples include age, sex at birth, and genetics. Age is the strongest known risk factor for dementia. Females are at an increased risk of developing dementia, and there are at least 75 genes that are associated with an increased risk of developing Alzheimer’s dementia (Bellenguez et al., 2022).
Modifiable risk factors include a range of lifestyle or behavioural factors (diet, exercise, social activities), as well as heart health, intellectual activities, and protecting your brain from injuries that can help reduce the risk of developing dementia. While we might not be able to cure dementia in the near future, by reducing lifetime exposure to modifiable risk factors we may be able to delay or even prevent dementia from occurring in many people.
The 2020 report of the Lancet Commission on Dementia Prevention, Intervention, and Care identified 12 modifiable risk factors that account for about 40% of dementia worldwide (Livingston et al., 2020). The report’s authors also took a life-course approach to identify specific actions that can be done over a lifetime. Examples of these actions are outlined in Figure 5.
In the past decade, we have seen further progress in our understanding of the risk factors for dementia. The evidence clearly suggests that the risk for late-life cognitive decline and dementia can be addressed by preventative actions.
The list of modifiable risk factors continues to grow with new research, yet significant gaps in knowledge remain, including differences across geographic locations, ethnic and cultural diversity, changes across the life course, biological mechanisms, and interactions between factors (Anstey et al., 2020).
Newer risk factors not included in earlier papers include sleep disturbance, atrial fibrillation, anxiety, cancer, carotid atherosclerosis, inflammatory markers, metabolic syndrome, peripheral artery disease, renal disease, serum uric acid, stroke, and pesticides (Anstey et al., 2019).
While there is a growing list of risk factors that can be labelled as modifiable, many Canadians may not be able to make these positive changes due to their personal situation and resources. These factors are only truly modifiable if the proper supports are provided by our communities, public health agencies, and other governmental organizations.
Combinations of risk factors tend to increase with age
Many of the risk factors associated with dementia onset are also closely tied to aging. As people grow older, they are at higher risk of developing a wide range of health issues, many of which have been linked to an increased risk of dementia.
In fact, dementia seldom travels alone; health conditions often occur together as people get older. In other words, “the problems of old age come as a package” (Fontana et al., 2014).
This is demonstrated by the common occurrence of multimorbidity—the presence of more than one chronic condition—in older Canadians. Using data from the Canadian Chronic Disease Surveillance System, analysts have demonstrated that over 50% of Canadians over the age of 70 have two or more chronic conditions.
Scientists have only just begun to study how having multiple risk factors raises the chance of developing dementia rather than just examining individual factors on their own. A 2019 study that reviewed the current scientific literature demonstrated that having three or more risk factors doubles the risk of developing dementia (Peters et al., 2019).
The evidence that overlapping or multiple risk factors further raises dementia risk is very strong. If the goal is to minimize dementia risk for an individual, all risk factor exposures must be minimized across their lifetime.
Researchers are also understanding more about the relationship between frailty and dementia. “Frailty” is used to describe a state of vulnerability when faced with a stressor. Frailty increases with the accumulation of multiple health deficits that can occur as we age. These deficits include symptoms, abnormal laboratory values, disease states, and disabilities (Clegg et al., 2013).
Studies have demonstrated that the more health deficits you have, the higher the risk for developing dementia (Ward et al., 2022). This line of research shows that a person’s overall health (and frailty level) is important to consider in understanding their dementia risk.
Recent research has begun to examine how overall health and frailty may be linked to a person’s ability to withstand changes in the brain that come with aging. This is an active area of research that may lead to a better understanding of brain health and resiliency in relation to dementia.
Promoting brain health
Brain health is related to both the integrity and biological functions of the brain, and also to the mental and cognitive functions that the brain produces (Stern, 2012). With aging, brains have to cope with numerous biological challenges that come from use over the years, along with a range of neurological disorders that can arise with time.
In contrast to the risk factors outlined above, epidemiological studies have found that there are also “protective factors” when it comes to dementia risk. These factors include a range of healthy habits that have been shown to reduce the risk of cognitive decline and dementia through actively influencing brain health.
Having more education, being physically active, staying connected with social activities, and eating healthy are just a few of the ways to improve brain health and protect against dementia risk. Refer to Box 3 for additional actions that can be taken to improve brain health.
Reducing more than one risk factor is key
Many researchers recommend multimodal interventions as the most likely way to delay the onset of dementia.
Multimodal interventions do not focus on just a single risk factor or one aspect of a person’s life. Instead, they work to address multiple risk factors for dementia in a single health promotion program.
One leading example of this work is the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (Ngandu et al., 2015). Researcher Miia Kivipelto and their team found success by creating an intervention that addressed diet, exercise, cognitive training and vascular risk monitoring. They found that this approach could improve or maintain cognitive functioning in older adults.
Based on the success of this research, a global network of 16 similar projects has been developed. Here in Canada, we have CAN-Thumbs Up—The Canadian Therapeutic Platform Trial for Multidomain Interventions to Prevent Dementia.
The Alzheimer Society partially funded this work which is focused on lifestyle and dementia risk factors in the Canadian context. Recruitment began in 2022 for their Brain Health Support Program Intervention, and more information can be found on the Canadian Consortium on Neurodegeneration in Aging website (ccna-ccnv.ca).
Box 3. Twelve actions for a healthier brain at any age
- Be physically active each day. Reduce sedentary time and move more. This can include all types of physical activities, including walking, running, weightlifting, gardening, yoga, tai chi, swimming, dancing, biking, team sports and yard work.
- Protect your heart. Monitor your blood pressure, cholesterol and diabetes closely. What’s good for the heart is also good for the brain.
- Stay socially active. Make sure to be engaged with friends and family. Maintain your social network and stay connected.
- Manage your medical conditions. Keep on top of your overall health. This is directly linked to your brain health and your ability to avoid dementia as you get older.
- Challenge your thinking. Take on mental leisure activities that you enjoy. Always try to learn new things, no matter what your age.
- Get a good night's sleep every night. Try to sleep 6 to 8 hours each night to help maintain your brain health.
- Have depression treated. Remember that depression is more than just feeling down. Seek help to improve the functioning of your brain.
- Avoid excessive alcohol intake. Limit your intake of wine, beer and other alcoholic beverages.
- Maintain your hearing. Use hearing aids if you need them. Protect your hearing from loud noises.
- Find meaning in life. Find a purpose to get out of bed each day. This is associated with better brain health and reduced dementia risk.
- Avoid all types of head injury. Steer clear of activities where you might put your brain at risk of harm.
- Adopt healthy behaviours. Make healthy food choices, reduce avoidable stress, quit or reduce smoking, and get regular check-ups with your doctor. All these actions will positively affect your brain health.
Even a small delay in dementia onset across Canada can make a significant difference nationally
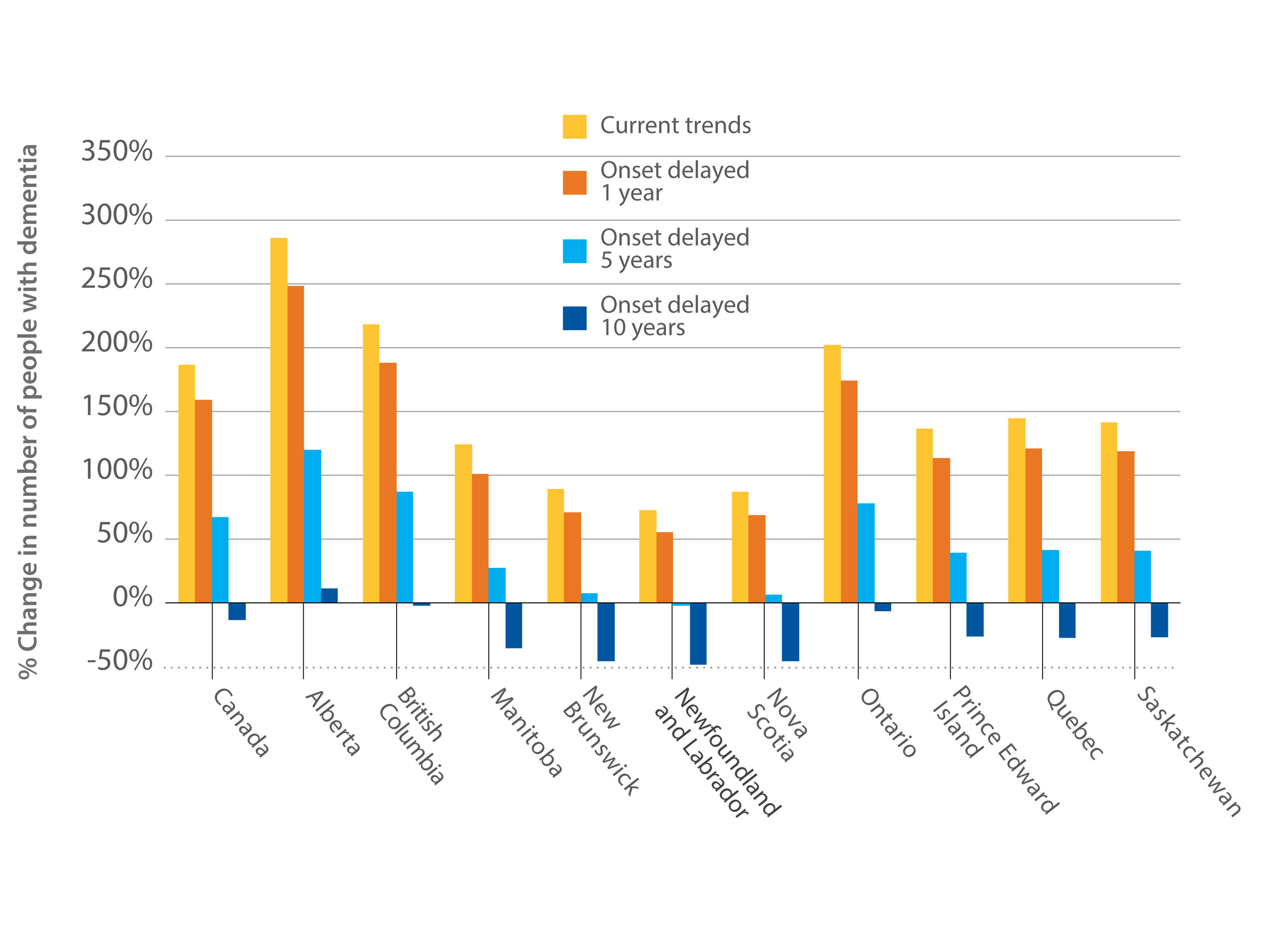
The Landmark Study developed three hypothetical scenarios where the onset of dementia in Canadians is delayed by 1, 5 or 10 years. The goal of these scenarios is to demonstrate what the effect would be on the Canadian population if we were able to improve risk reduction efforts for dementia and delay its onset across our population.
For these three scenarios, we made no specific assumptions about how to achieve such reductions (i.e., change in risk factors). These scenarios are essentially adjustments to the simulation model where the risk of dementia onset is shifted for everyone. The goal of these hypothetical scenarios is to understand what the population-level effects might be if we had successful population-level interventions.
All three hypothetical scenarios demonstrate the power of risk reduction at a national level.
Even a delay of 1 year could result in almost 500,000 fewer new cases by 2050; this would make a huge difference in national dementia rates over the next three decades (Table 7). If the onset of dementia could be delayed by 10 years, over 4 million new cases of dementia could be avoided by 2050 (Table 7).
In the scenario with a 10-year delay, there would be slightly fewer people living with dementia in 2050 compared to 2020 (Table 8). While a 10-year shift in onset may seem unreasonable based on the science at this time, it is not impossible. Some research has already demonstrated that maintaining a cognitively active lifestyle in old age (e.g., reading, visiting libraries, writing, playing games) may delay the onset of Alzheimer’s dementia by as much as 5 years (Wilson et al., 2021).
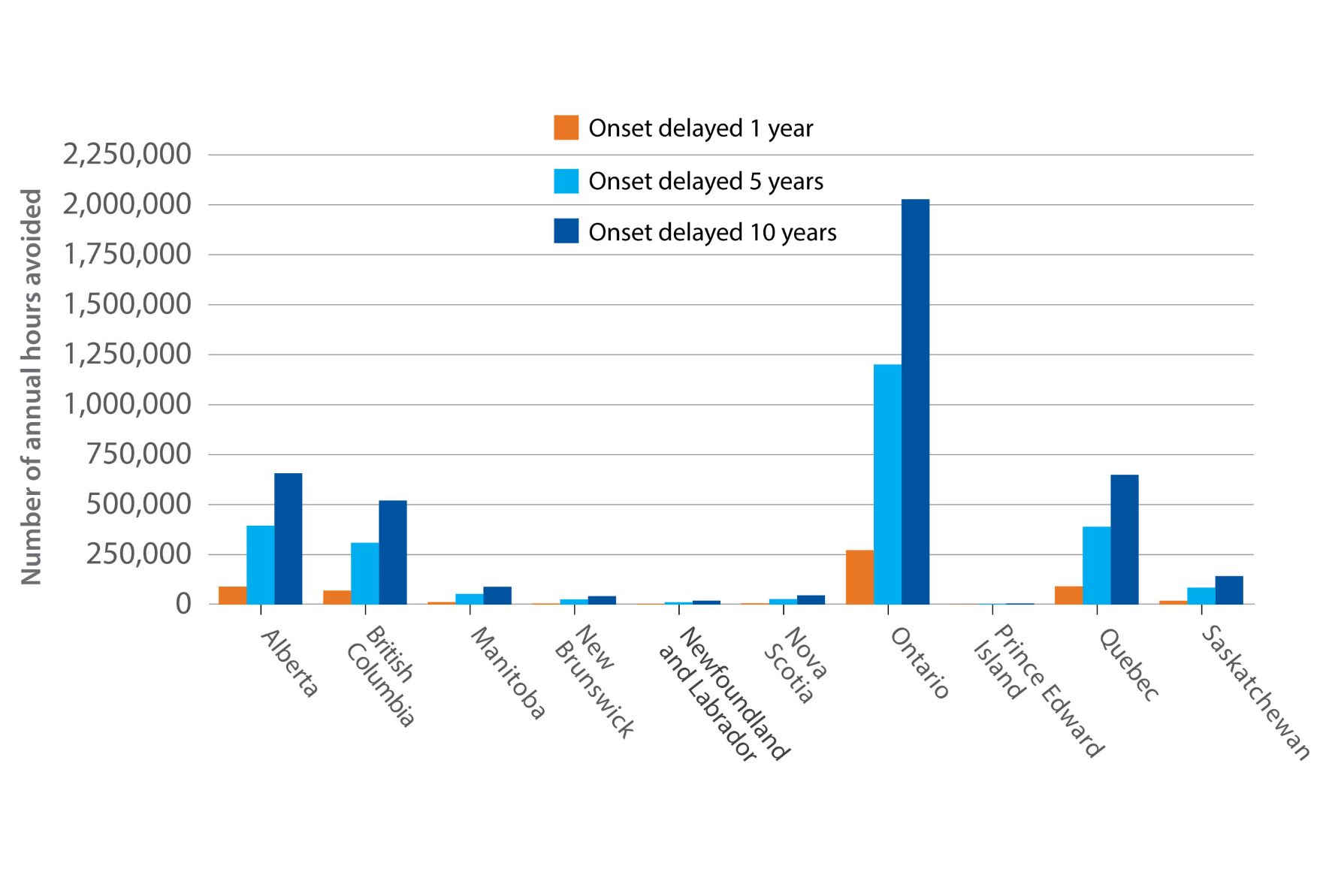
Delaying the onset of dementia could also have an enormous impact on caregiving for people living with dementia in Canada (Table 9). A 10-year delay could reduce the number of caregiving hours needed by almost 1 billion hours per year (Figure 7).
High-risk individuals versus whole-population approaches to risk reduction
When focusing on risk factors for dementia, interventions and actions are often examined through the lens of the individual. It is important to learn about what individuals can do for themselves and what health-care providers can do to support individual health during the aging process.
However, there also needs to be some focus on what can be done at a population level in Canada to address the challenge of dementia. While we might not be able to completely prevent dementia, the science is quite clear that dementia risk can be modified. From a population perspective, this is of key importance, as even the slightest delays in dementia onset can have a huge influence on national statistics.
At the population level, there are two broad approaches to dementia risk reduction:
- The high-risk approach directs interventions at people identified as being at a higher risk of dementia. This targeted approach uses education and interventions to help people respond to their elevated risk.
- The whole-population approach aims to reduce everyone’s risk across society. This could include actions such as new legislation, investments in infrastructure, and other broad approaches at a community, provincial or federal level.
Most risk reduction activities take the high-risk approach, with interventions designed to focus on older individuals at the greatest risk of developing dementia.
However, if we only focus on at-risk individuals, it is unlikely that we will be able to significantly reduce the overall strain of dementia across Canada in the long-term due to the following reasons (Walsh et al., 2022):
- Dementia and its modifiable risk factors are very common in Canada. At-risk approaches will miss a large number of people who will go on to develop the condition.
- Dementia occurs as the result of cumulative exposure to multiple risk factors across the life course. Whole-population approaches that influence the environments in which people live, work and play have greater potential to reduce overall dementia risk.
- Dementia has been shown to be closely associated with socio-economic status. Whole-population approaches could be designed to reduce inequalities and engage people of all backgrounds.
High-risk and whole-population approaches are complementary, and both are needed if we are to effectively tackle the challenge of dementia in Canada.
Chapter 4: Differences in dementia rates across regions of Canada
The growth in dementia cases will not be uniform across the country
All regions of Canada are expected to see an increase in the number of people with dementia if current trends continue. However, the growth in dementia cases will not be uniform across the country.
Dementia will affect the provinces differently over the next 30 years. Differences in age distributions, migration patterns, and the prevalence of risk factors combine to produce specific challenges, needs, and overall numbers of people living with dementia for each province. Unfortunately, insufficient data was available to study the Yukon, the Northwest Territories, or Nunavut.
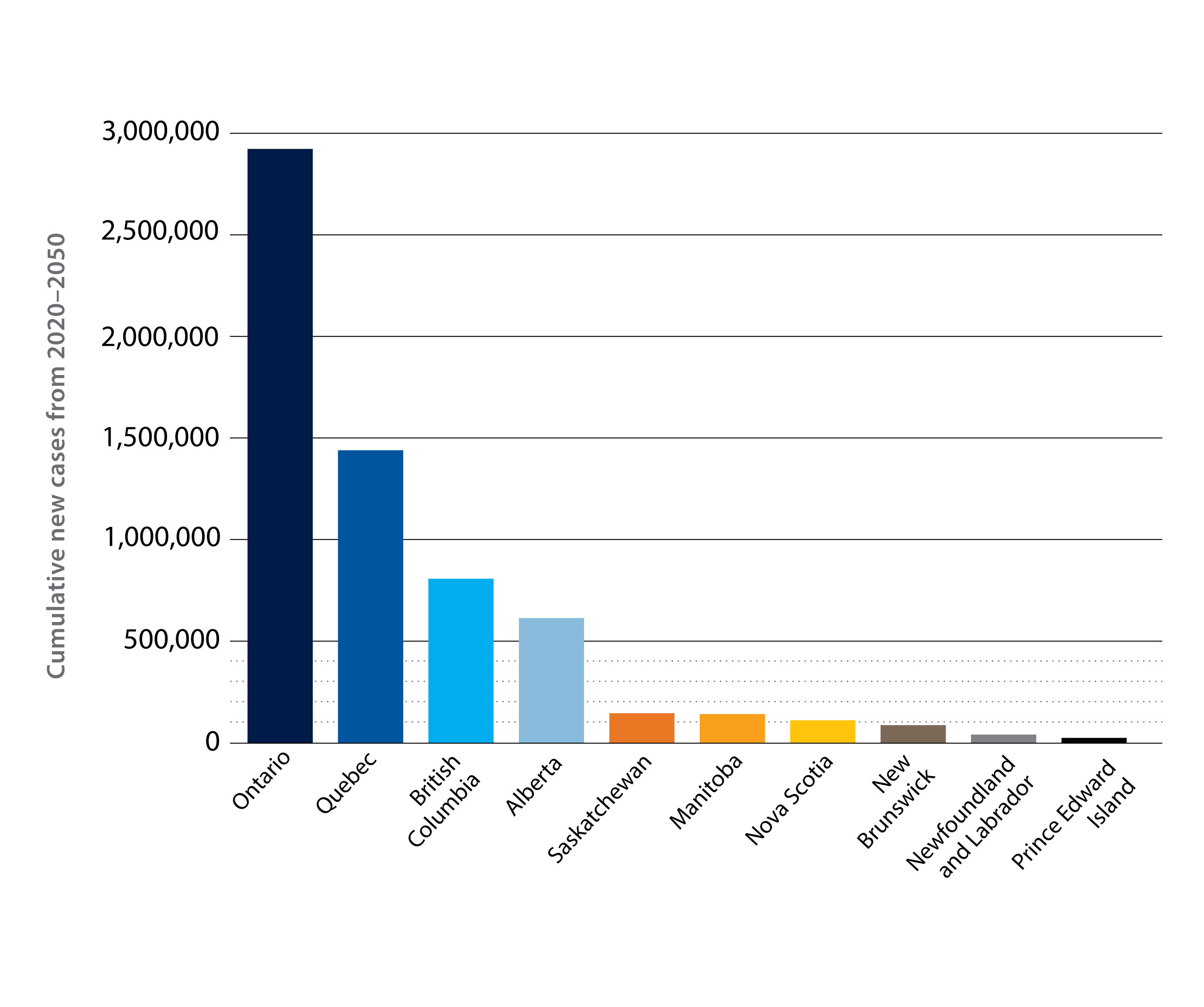
Based on the data that was used for the Landmark Study, the expected percentage increases of people living with dementia vary considerably across the 10 provinces (Figure 8).
Largest percentage increases will occur in Ontario, Alberta, and British Columbia
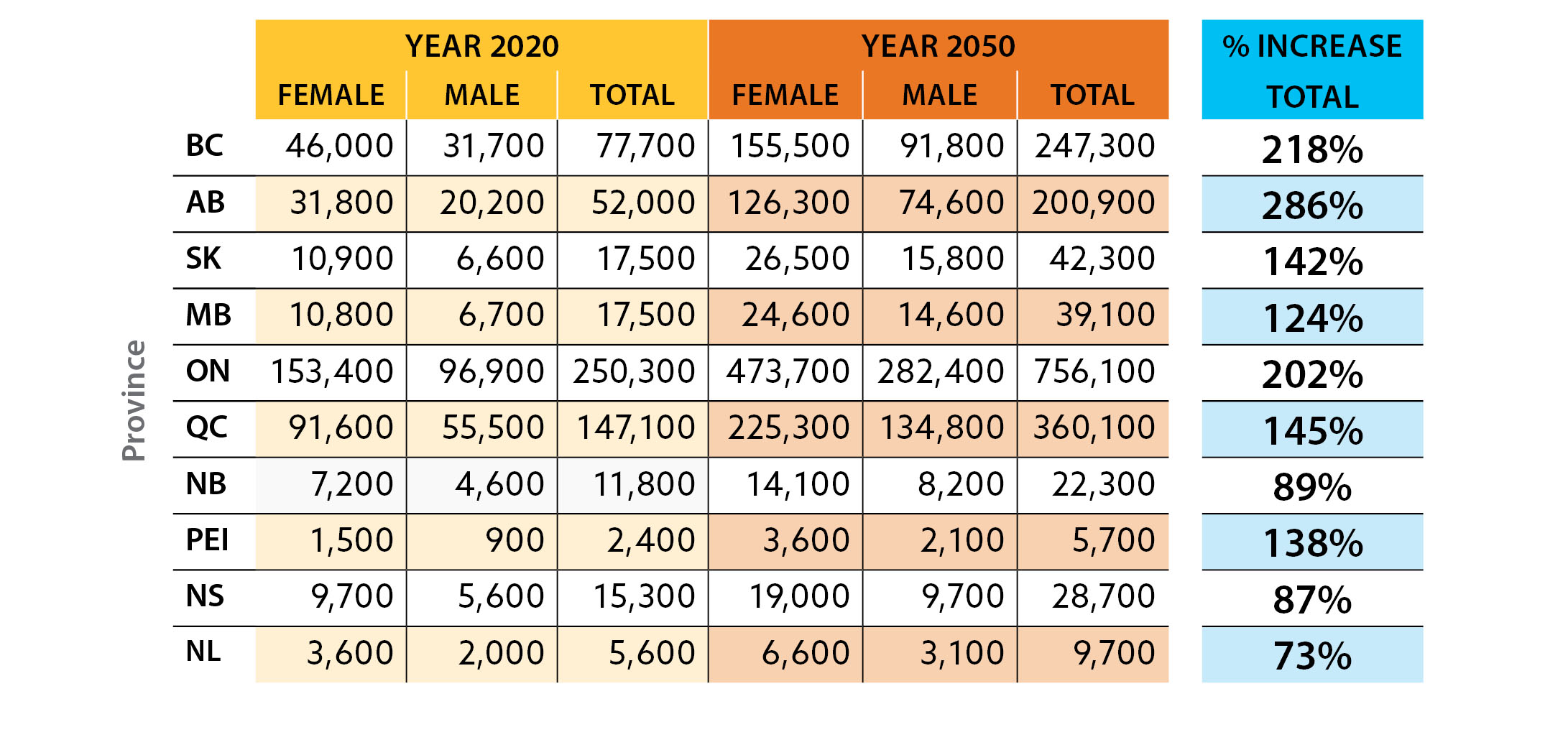
Faster growing and younger provinces, such as Ontario, Quebec, British Columbia and Alberta, will have the most significant increases in dementia by 2050 (Figure 8, Table 10).
Ontario, with a 202% increase over the three decades, is projected to have the most new cases by 2050: 1.5 million new cases of Alzheimer's dementia; 680,000 new cases of vascular dementia; and 780,000 new cases of other types of dementia.
Alberta and British Columbia are expected to have greater percentage increases in people living with dementia. Alberta will see a 286% increase in the number of people living with dementia from 2020 to 2050. For British Columbia, this increase will be 218%.
These large increases in Ontario, Alberta, and British Columbia are driven by higher growth rates and faster-aging populations than other provinces (Figure 9).
Quebec is expected to have the second-highest increase in the number of people with dementia (2020: 147,000 people living with dementia; 2050: 360,200), but stands to be below the national average in terms of percentage increase over the three decades (Quebec: 145% increase from 2020–2050; Canada: 187%).
While the Atlantic provinces have, on average, older populations than other parts of the country, their much slower population growth limits the rate of dementia growth. However, substantial growth in dementia numbers is still expected from 2020 to 2050:
- New Brunswick: 89% increase
- Prince Edward Island: 138% increase
- Nova Scotia: 87% increase
- Newfoundland and Labrador: 73% increase
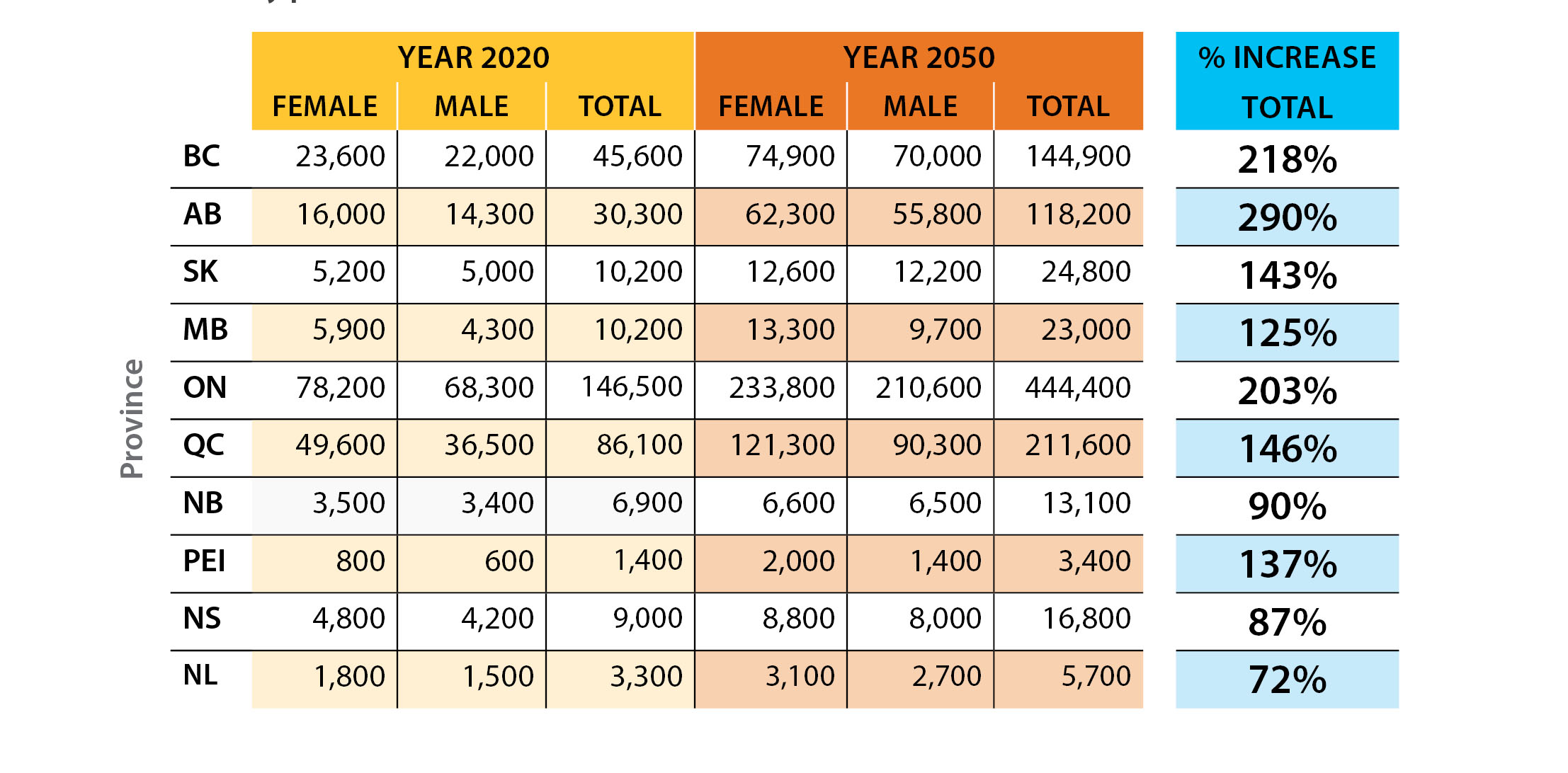
Caregiving needs across the provinces
Alberta is expected to see the largest percentage increase in the number of care partners for people living with dementia (290% increase, Table 11) and the number of hours of unpaid caregiving (302% increase) compared to the rest of the country.
On average, Canada will see a 188% increase in the total number of care partners and a 193% increase in the number of hours of unpaid caregiving.
Delay in dementia onset across the provinces
Our study also examined the potential impact of delaying dementia onset at the provincial level.
Delaying onset by 10 years would have different impacts on each province and territory. Projecting to 2050, the Atlantic provinces would experience the largest decreases in dementia. Ontario, British Columbia and Alberta would see their 2050 numbers remain similar to those in 2020, completely changing the trajectories projected without a delay (Figure 10).
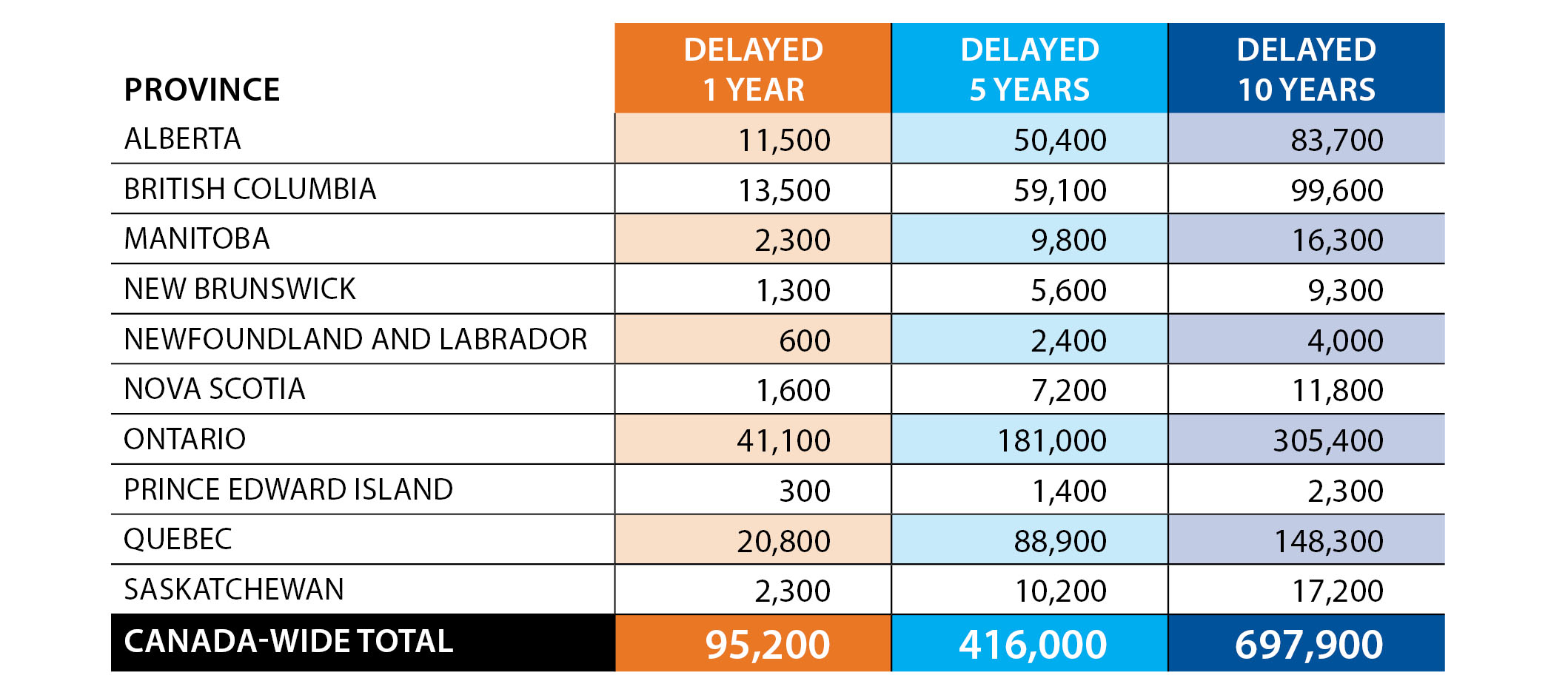
Likewise, the impacts on care partners in different provinces and territories would vary. With a 10-year dementia delay, by 2050, Ontario would need 305,400 fewer care partners and 440 million fewer hours of unpaid caregiving (equivalent to 220,000 full-time jobs). In this scenario, even a small province like Prince Edward Island would need 2,300 fewer care partners in 2050 (Table 12).
Chapter 5: Finding the best path forward
Summary
Dementia will continue to be a growing issue in Canada, with the number of people living with some form of dementia projected to triple over the next 30 years. If current trends continue, all regions of the country will see a dramatic increase in the number of people with dementia and the demands placed on care partners.
All people in Canada have a role to play in this challenge of finding a better path forward.
Based on current trends, 1.7 million people in Canada could be living with dementia by 2050, with over 6.3 million diagnoses of dementia occurring from 2020 to 2050.
By 2050, over 650,000 family and friend care partners will be needed to support people living with dementia. This amount of caregiving is expected to total almost 1.4 billion hours annually, equivalent to 690,000 full-time jobs.
These surging dementia caregiving needs will pose a big challenge to families, friends and other people who provide unpaid care for people living with dementia. The challenge is only partly due to the hours required. Caregiving demands occur for most people when they are 45 to 65, influencing workforce participation, personal finances, pension earnings and overall economic activity. When caregiving is performed by spouses or partners, they may have their own age-associated health challenges. For care partners who are 35 or younger, it can be challenging to launch a career, continue an educational path, or raise young children.
Measures which bring about even small delays in the onset of dementia could significantly reduce the demand for dementia care.
The Landmark Study model demonstrates that if the onset of dementia is delayed by 1 year, almost 500,000 cases of dementia in Canada could be avoided over the next 30 years. If the incidence of dementia could be delayed by 10 years, over 4 million diagnoses of dementia could be avoided, and most regions of the country would see fewer people living with dementia in 2050 than today.
While all regions of Canada are expected to see a substantial increase in the number of people living with dementia if current trends continue, some provinces will experience greater change. Provinces with higher growth rates and faster-aging populations (such as Alberta, Ontario and British Columbia) are expected to see the number of people with dementia increase much faster than the other parts of Canada.
Opportunities to improve the path
While a cure or an effective treatment for dementia has not yet been discovered, we can take a wide range of actions to create positive outcomes for people living with dementia and their care partners.
All people in Canada have a role to play in this challenge. As a result, these sections have been organized to address the following various perspectives: What can Alzheimer Societies do? What can health-care systems do? What can the federal, provincial/territorial and municipal levels of government do? What can researchers do? What can individual Canadians do? For all of these groups, it is important that this work is done collaboratively with people living with dementia and their care partners.
What can Alzheimer Societies do?
- Reduce stigma and raise public awareness about dementia so that all Canadians know about dementia-friendly community programming and the IG Wealth Management Walk for Alzheimer's.
- Grow supports and services to fill the gaps in health care through the First Link® system navigation program, National Dementia Infoline, provincial and regional dementia infolines, Minds in Motion and other invaluable local programs.
- Increase funding for out-of-the-box research that explores radical new ways to advance our knowledge of dementia and enhances the quality of life of people living with dementia and their care partners.
- Continue building relationships and resources for diverse communities across Canada.
- Engage people living with dementia and their care partners in all aspects of advocacy and programming in keeping with "nothing for us, without us."
- Collaborate with other organizations on issues related to dementia and dementia care.
What can health-care systems do?
- Provide primary care clinicians with:
- Better education on timely detection of dementia symptoms, diagnosis, and particularly ongoing care.
- Better access to the right tools to diagnose dementia and provide ongoing management.
- Support for medication review and deprescribing initiatives that are readily accessible.
- Education on risk reduction approaches to dementia.
- Changes to fee structures so that clinicians have the right time allocation and remuneration to provide proper support to people living with dementia and their care partners.
- Provide training to a broader circle of allied health professionals who can support management of dementia, including pharmacists, nurses, social workers and personal support workers.
- Increase the dementia workforce and the resources available to all allied health professionals who care for people living with dementia, regardless of where they live in Canada.
- Grow capacity for dementia-specialized community clinics, community and home care systems, and long-term care. Home and community care is the more affordable and requested option by people living with dementia.
- Recognize the specific needs and supports of care partners and people living with dementia to improve care.
- Work to address barriers for access to care among underserved populations, including rural communities, Indigenous Peoples, and other diverse communities.
- Require that health records indicate mild cognitive impairment and early, middle or late-stage dementia.
- Provide effective support for dementia care partners through primary care and health professionals. This includes connecting care partners with local Alzheimer Societies and other local supports, asking about care partner stress, making sure that a primary care partner is identified, assessing care partners prior to hospital discharge, and considering care partner status when determining care transition plans.
What can the federal government do?
- Cost out and fully fund the National Dementia Strategy to optimize the work done toward the three national objectives: (1) prevent dementia; (2) advance therapies and find a cure; (3) improve quality of life of people living with dementia and care partners.
- Furthermore, develop key performance indicators, benchmarks or metrics for the strategy so that the successes and failures can be evaluated.
- Increase investments in dementia research to reach the goal set in the National Dementia Strategy of 1% of dementia care (approximately $105 million annually), including work in health systems and health promotion.
- Actively work to reduce stigma against dementia through national awareness campaigns, and promote measures toward creating dementia-friendly communities.
- Support the development of national dementia clinical guidelines, and fund the development of clinical tools related to dementia care.
- Empower and fund the Public Health Agency of Canada to do what is called "dementia surveillance"—that is, making sure every case of dementia in Canada is counted and tracked.
- Recognize modifiable risk factors for dementia and integrate health promotion strategies across non-communicable diseases of aging, including neurological disorders, heart disease, cancer, and diabetes.
- Provide additional targeted funding for technological solutions to the challenges that come with dementia, clinical dementia care, and caregiving.
- Enhance strategies to improve the mental health of older Canadians, with the specific targeting of reducing depression in people over the age of 65.
- Support implementation of care partner leave more widely—put it in Canadian law—including paid leave for long-term conditions.
What can provincial and territorial governments do?
- Create new community care and long-term care spaces that are dementia friendly, and encourage dementia-friendly community developments.
- Plan for increases in spending for home care, social supports, and long-term care to match the expected increases in the number of people living with dementia and their care partners.
- Improve access to memory clinics, with additional focus on underserved urban regions and rural areas.
- Take a World Health Organization “Health in All Policies” approach to public policy that systematically takes into account the health implications of decisions, seeks synergies, and avoids harmful health impacts of all new provincial policies.
- Continue to improve efforts by public health agencies in the following areas: prevention and treatment of vascular conditions; discouraging smoking and heavy alcohol use; and encouraging healthy lifestyles.
- Develop policies that encourage social, cognitive and physical activity across the life course for all. This process should include robust efforts to effectively address the social determinants of health.
- Enhance strategies to improve the mental health of older adults, with the specific targeting of reducing depression in people over the age of 65.
- Improve education for all ages—from primary school to adult education—to enhance the brain health of all Canadians.
- Consider how annual brain health checkups for people over 50 might work within each province or territory. The science of brain health has evolved to a point where biomarkers and imaging technologies could be used in health system-level risk reduction activities.
- Support federal efforts in dementia surveillance—provinces must urgently start to enhance the tracking of diagnoses more accurately.
- Create policies and processes that support culturally safe dementia care and public health initiatives for people of all backgrounds, including Indigenous Peoples, Black Canadians, and other racialized and intersectionally oppressed groups.
- Destigmatize and enhance supports for younger care partners.
- Respond to care partner challenges, specifically in rural and remote settings where supports are often lacking.
- Support workplaces in providing flexible supports for employed care partners.
- Build up a system of interventions designed to assist care partners that may include:
- Case management
- Psychoeducational approaches
- Counselling
- Psychotherapeutic approaches
- Respite
- Support groups
- Multicomponent approaches
- Healthy living
What can municipal governments do?
- Work toward developing age-friendly and dementia-friendly action plans.
- Work closely with public health units to support their messaging and programming around brain health.
- Support intergenerational social interaction and physical activity for all ages through suitably funded and maintained parks and recreation programs, community centres, and public health programs.
- Reduce air pollution and encourage more green space.
- Support existing community cultural organizations in delivering brain health programs appropriate to their members and target audiences.
- Support accessibility initiatives in urban planning and design that include clear wayfinding signage and transit accessibility.
- Consider health impacts in all policy making, and support health promotion efforts by other levels of government.
- Encourage all city staff to take a dementia-friendly course via alzheimer.ca/DementiaFriendlyCanada.
- Fund local support networks for people living with dementia and their care partners.
- Encourage more dementia-friendly spaces and parks and recreation programming.
What can researchers do?
- Include people living with dementia and their care partners in research projects, as part of the research team and as study participants.
- Embrace a range of dementia research, including fundamental bio-medical and clinical research, dementia in health systems and services, dementia in populations, the societal and cultural dimensions of dementia, and the environmental influences on dementia.
- Support an integrated approach to dementia research that brings together researchers, health-care providers and policy-makers with industry and patient groups from across the country.
- Continue to conduct studies to understand protective effects, risk factors, and interventions for dementia over the life course.
- Support brain health-oriented research, such as further investigation into the factors that lead to resiliency and cognitive/brain reserves.
- Ensure that dementia research populations reflect the diversity in our Canadian population. Increase recruitment of heterogeneous samples to improve our understanding of differences such as socio-economic status, race, ethnicity, language, disability, and gender.
- Continue research on the COVID-19 pandemic and its association with dementia outcomes.
- Work to develop new insights on the care needs of people living with dementia, the needs of care partners, and ways to improve the health and social systems that support them.
- Study how the social determinants of health (i.e., social and environmental attributes beyond an individual’s control) affect the risk of developing dementia and the well-being of people living with dementia and their care partners.
- Foster interdisciplinary collaborations to tackle the complex problems that exist in dementia research. For example, quantitative research projects may benefit by including data scientists with expertise in areas like machine learning, artificial intelligence, or other modern data science approaches.
- Conduct research on technological and non-technological innovations aimed at improving dementia care (e.g., assistive technologies, virtual reality applications, human-based interventions). Some of this work should include harnessing sensor technology and the Internet of Things for applications in dementia management and care (e.g., remote monitoring of appliances, tracking of biometrics, medication management).
- Identify common causes of hearing loss and head trauma (e.g., occupational exposures), and work to reduce exposure to these risk factors (which have been shown to elevate dementia risk as individuals age).
- Conduct health system research on implementing better coordination and integrated care that is patient-centred and dementia friendly.
What can individuals in Canada do?
- Support care partners within your families and social networks.
- Grow your awareness about dementia and how it impacts people, support dementia research and enhanced services for people with dementia, and be prepared to act as a care partner.
- Advocate for your community to become dementia friendly and for more funding for the National Dementia Strategy or your provincial dementia strategy.
- Access programs available through your local Alzheimer Society if you or anyone you know is concerned about or living with dementia.
- No matter what your age group, from youth to older adults, actively improve your brain health and take dementia risk reduction measures:
- Be physically active each day.
- Protect your heart.
- Stay socially active.
- Manage your medical conditions.
- Challenge your thinking.
- Get a good night’s sleep every night.
- Have depression treated.
- Avoid excessive alcohol intake.
- Maintain your hearing.
- Find meaning in life.
- Avoid all types of head injury.
- Adopt a healthy lifestyle by making healthy food choices, reducing avoidable stress, quitting or reducing smoking, and getting regular check-ups with your doctor.
References and Acknowledgements
- References
-
Andrew, M. K., & Tierney, M. C. (2018). The puzzle of sex, gender and Alzheimer’s disease: Why are women more often affected than men? Women’s Health. https://doi.org/10.1177/1745506518817995
Angeles, R. C., Berge, L. I., Gedde, M. H., Kjerstad, E., Vislapuu, M., Puaschitz, N. G., & Husebo, B. S. (2021). Which factors increase informal care hours and societal costs among caregivers of people with dementia? A systematic review of Resource Utilization in Dementia (RUD). Health Economics Review, 11(1), 37–37. https://doi.org/10.1186/s13561-021-00333-z
Anstey, K. J., Ee, N., Eramudugolla, R., Jagger, C., & Peters, R. (2019). A systematic review of meta-analyses that evaluate risk factors for dementia to evaluate the quantity, quality, and global representativeness of evidence. Journal of Alzheimer’s Disease, 70(s1), S165–S186. https://doi.org/10.3233/JAD-190181
Anstey, K. J., Peters, R., Zheng, L., Barnes, D. E., Brayne, C., Brodaty, H., Chalmers, J., Clare, L., Dixon, R. A., Dodge, H., Lautenschlager, N. T., Middleton, L. E., Qiu, C., Rees, G., Shahar, S., & Yaffe, K. (2020). Future directions for dementia risk reduction and prevention research: An international research network on dementia prevention consensus. Journal of Alzheimer’s Disease, 78(1), 3–12. https://doi.org/10.3233/JAD-200674
Bellenguez, C., Küçükali, F., Jansen, I. E., Kleineidam, L., Moreno-Grau, S., Amin, N., Naj, A. C., Campos-Martin, R., Grenier-Boley, B., Anade, V., Holmans, P. A., Boland, A., Damotte, V., van der Lee, S. J., Costa, M. R., Kuulasmaa, T., Yang, Q., de Rojas, I., Bis, J. C., … Ahmad, S. (2022). New insights into the genetic etiology of Alzheimer’s disease and related dementias. Nature Genetics, 54(4), 412–436. https://doi.org/10.1038/s41588-022-01024-z
Bergvall N., Brinck, P., Eek D., Gustavsson, A., Wimo, A., Winblad, B., & Jönsson, J. (2011). Relative importance of patient disease indicators on informal care and caregiver burden in Alzheimer's disease. International Psychogeriatrics, 23(1), 73–85. https://doi.org/10.1017/S1041610210000785
Canadian Institute for Health Information. (2018a). Dementia in home and community care. https://www.cihi.ca/en/dementia-in-canada/dementia-care-across-the-health-system/dementia-in-home-and-community-care
Canadian Institute for Health Information. (2018b). Unpaid caregiver challenges and supports. https://www.cihi.ca/en/dementia-in-canada/unpaid-caregiver-challenges-and-supports
Chambers, L. W., Bancej, C., & McDowell, I. (2016). Prevalence and monetary costs of dementia in Canada: Population health expert panel. Alzheimer Society of Canada. https://admin.alzheimer.ca/sites/default/files/documents/Prevalence-and-costs-of-dementia-in-Canada_Alzheimer-Society-Canada.pdf
Clegg, A., Young, J., Iliffe, S., Rikkert, M. O., & Rockwood, K. (2013). Frailty in elderly people. The Lancet (British Edition), 381(9868), 752–762. https://doi.org/10.1016/S0140-6736(12)62167-9
Fisher, S., Manuel D. G., Hsu, A. T., Bennett, C., Tuna, M., Eddeen, A. B., Sequeira, Y., Jessri, M., Taljaard, M., Anderson, G. M., & Tanuseputro, P. (2021). Development and validation of a predictive algorithm for risk of dementia in the community setting. Journal of Epidemiology and Community Health, 75, 843–853. http://jech.bmj.com/content/75/9/843.abstract
Fontana, L., Kennedy, B., Longo, V., Seals, D., & Melov, S. (2014). Medical research: Treat ageing. Nature, 511, 405–407. https://doi.org/10.1038/511405a
Huang, H. L., Shyu, Y. I., Chen, M. C., Huang, C. C., Kuo, H. C., Chen, S. T., & Hsu, W. C. (2015). Family caregivers' role implementation at different stages of dementia. Clinical interventions in aging, 10, 135–146. https://doi.org/10.2147/CIA.S60574
Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., Brayne, C., Burns, A., Cohen-Mansfield, J., Cooper, C., Costafreda, S. G., Dias, A., Fox, N., Gitlin, L. N., Howard, R., Kales, H. C., Kivimäki, M., Larson, E. B., Ogunniyi, A., … Mukadam, N. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet (British Edition), 396(10248), 413–446. https://doi.org/10.1016/S0140-6736(20)30367-6
Ngandu, T., Lehtisalo, J., Solomon, A., Levälahti, E., Ahtiluoto, S., Antikainen, R., Bäckman, L., Hänninen, T., Jula, A., Laatikainen, T., Lindström, J., Mangialasche, F., Paajanen, T., Pajala, S., Peltonen, M., Rauramaa, R., Stigsdotter-Neely, A., Strandberg, T., Tuomilehto, J., Soininen, H., … Kivipelto, M. (2015). A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. The Lancet (British Edition), 385(9984), 2255–2263. https://doi.org/10.1016/S0140-6736(15)60461-5
Ory, M. G., Hoffman R., Yee J. L., Tennstedt, S., & Schulz, R. (1999). Prevalence and impact of caregiving: A detailed comparison between dementia and nondementia caregivers. Gerontologist, 39, 177–185. https://doi.org/10.1093/geront/39.2.177
Peters, R., Booth, A., Rockwood, K., Peters, J., D'Este, C., & Anstey, K. J. (2019). Combining modifiable risk factors and risk of dementia: A systematic review and meta-analysis. BMJ open, 9(1), e022846. https://doi.org/10.1136/bmjopen-2018-022846
Pinquart, M., & Sörensen, S. (2003). Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. The Journals of Gerontology: Series B, 58(2), 112–28. https://doi.org/10.1093/geronb/58.2.P112
Richardson, T. J. (2013). Caregiver health: Health of caregivers of Alzheimer’s and other dementia patients. Current psychiatry reports, 15(7). https://doi.org/10.1007/s11920-013-0367-2
Statistics Canada. (2020, November 24). The experiences and needs of older caregivers in Canada. https://www150.statcan.gc.ca/n1/pub/75-006-x/2020001/article/00007-eng.htm
Statistics Canada. (2022a, April 27). In the midst of high job vacancies and historically low unemployment, Canada faces record retirements from an aging labour force: Number of seniors aged 65 and older grows six times faster than children 0-14. https://www150.statcan.gc.ca/n1/daily-quotidien/220427/dq220427a-eng.htm
Statistics Canada. (2022b, January 14). Caregiving by the hours, 2018. https://www150.statcan.gc.ca/n1/pub/11-627-m/11-627-m2021074-eng.htm
Stern, Y. (2012). Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurology, 11(11), 1006–1012. https://doi.org/10.1016/S1474-4422(12)70191-6
Teahan, A., Lafferty, A., McAuliffe, E., Phelan, A., O’Sullivan, L., O’Shea, D., & Fealy, G. (2018). Resilience in family caregiving for people with dementia: A systematic review. International Journal of Geriatric Psychiatry, 33(12), 1582–1595. https://doi.org/10.1002/gps.4972
Walsh, S., Govia, I., Wallace, L., Richard, E., Peters, R., Anstey, K. J., & Brayne, C. (2022). A whole-population approach is required for dementia risk reduction. The Lancet. Healthy Longevity, 3(1), e6–e8. https://doi.org/10.1016/S2666-7568(21)00301-9
Ward, D. D., Ranson, J. M., Wallace, L. M. K., Llewellyn, D. J., & Rockwood, K. (2022). Frailty, lifestyle, genetics and dementia risk. Journal of Neurology, Neurosurgery and Psychiatry, 93(4), 343–350. http://dx.doi.org/10.1136/jnnp-2021-327396
Wilson, R. S., Wang, T., Yu, L., Grodstein, F., Bennett, D. A., & Boyle, P. A. (2021). Cognitive activity and onset age of incident Alzheimer disease dementia. Neurology, 97(9), e922–e929. https://doi.org/10.1212/WNL.0000000000012388
Yu, D., Cheng, S. T., & Wang, J. (2018). Unravelling positive aspects of caregiving in dementia: An integrative review of research literature. International Journal of Nursing Studies, 79, 1–26. https://doi.org/10.1016/j.ijnurstu.2017.10.008
Zhu, C. W., Scarmeas, N., Ornstein, K., Albert, M., Brandt, J., Blacker, D., Sano, M., & Stern, Y. (2015). Health-care use and cost in dementia caregivers: Longitudinal results from the Predictors Caregiver Study. Alzheimer’s & Dementia, 11(4), 444–454. https://doi.org/10.1016/j.jalz.2013.12.018
- Acknowledgements
-
The Landmark Study is based on a project conducted by the Canadian Centre for Economic Analysis (CANCEA) on behalf of the Alzheimer Society of Canada (ASC). This project was made possible by contributions from our generous donors.
ASC would like to say a special thank you to its Advisory Group of care partners and people living with dementia, subject matter experts, and citizen reviewers who have graciously provided their thoughts and guidance for the report.
Vision: The Landmark Study series was developed under the overall guidance and conceptualization of Dr. Saskia Sivananthan and Kevin Noel.
Project coordination and editing: The writing and conceptualization of this report was led by Dr. Joshua J. Armstrong. The team that coordinated the development of the report comprised Dr. Josée Guimond, Leah Sandals, Bob Neufeld, Nathan Christie, Stephe Perry, Jona John, Taiwo Akintade and Sabrina Bayne. The help of Gina D'Souza, Sian Lockwood, Camryn Berry, Anita Zaferani, Jacob Maher and Robert Guglielmin was also essential.
Technical contributions and review: Valuable input was received from staff at ASC, provincial partners and dementia experts, which has been central to the development of this report. Production team: technical editing by Laura Van Alphen; design by Naomi Shacter Graphic Design (NSG:D); French adaptation by Sébastien Kabacinski of Sigma Translations; French editing by Marie-Camille Lalande; and French proofreading by Caroline Couillard.
Subject matter experts: ASC gratefully acknowledges the contributions of the individuals listed here. Their expert opinion was essential in the creation of this document.
- Nicole D. Anderson, Baycrest Academy for Research & Education
- Melissa Andrew, Dalhousie University
- Jennifer Bethell, University of Toronto
- Darrell Bricker, Ipsos Public Affairs
- Larry W. Chambers, McMaster University
- Feng Chang, University of Waterloo
- Roger A. Dixon, University of Alberta
- Vivian Ewa, University of Calgary
- John Fisk, Dalhousie University
- Shannon Freeman, University of Northern British Columbia
- Serge Gauthier, McGill University
- Allan Grill, Markham Stouffville Hospital
- Andrea Gruneir, University of Alberta
- Vladimir Hachinski, Western University
- Dawn Hemingway, University of Northern British Columbia
- David Hogan, University of Calgary
- Lillian Hung, University of British Columbia
- Robert Laforce, Université Laval
- Monica Lavoie, Université Laval
- Ruth Ann Marrie, University of Manitoba
- Colleen Maxwell, University of Waterloo
- Carrie McAiney, University of Waterloo
- Laura Middleton, University of Waterloo
- Graciela Muniz, Terrera University of Edinburgh
- Megan O'Connell, University of Saskatchewan
- Kenneth Rockwood, Dalhousie University
- Dallas Seitz, University of Calgary
- Paul Smetanin, Canadian Centre for Economic Analysis
- David Stiff, Canadian Centre for Economic Analysis
- Suzanne Tyas, University of Waterloo
- Cornelia van Ineveld, University of Manitoba
- Isabelle Vedel, McGill University
- Christina Wolfson, McGill University
Appendix: Summary of microsimulation modelling methods
The Landmark Study uses the socio-economic statistical analysis platform from the Canadian Centre for Economic Analysis (CANCEA) to model and estimate the challenge of dementia in the Canadian population over the next 30 years.
In the model, “agents” are used as statistical representations of persons. Each agent is associated with several demographic characteristics (including age, sex and ethnicity) which match those of the Canadian population, as informed by publicly available data from Statistics Canada. The initial state of the population is established with age- and sex-specific prevalence of long-term health conditions, such as heart disease, smoking, hearing loss, or low level of physical activity, and the comorbidities between them.
The model simulates the agents and their interactions over time as they age and pass through various states, such as dementia diagnosis, hospitalization and death. While similar to other microsimulation models like the Population Health Model (POHEM) (Hennessy, et al., 2015), CANCEA’s platform can run at the individual level, include interactions and connections between agents (such as family structure), and can include extensive economic accounts.
This allows the single model to provide estimates and forecasts over time for measures of health (incidence, prevalence, mortality) and economics (direct and indirect health-care costs, government revenue lost, caregiver costs). This allows researchers to compare the impact of dementia across different segments of the population, namely by sex and ethnicity, and to identify populations particularly vulnerable to dementia in Canada.
The section below provides an overview of the approach used by CANCEA in the Alzheimer Society of Canada Dementia Model.
Model overview
The model is based on the simulation of a statistical representation of the Canadian population at the
individual level. Each person (agent) in the model has extensive data associated with it including the
following:
Demographics
- Date of birth
- Sex at birth
- Location of residence (census subdivision level)
- Ethnicity
- Family members
Health state
- Diabetes
- Obesity
- Stroke
- Diet
- Hypertension
- Mood/anxiety disorders
- Hearing loss
- Level of physical activity
- Alzheimer’s dementia*
- Vascular dementia
- Other forms of dementia
The model tracks the population through their lives and interactions, changing their state according to rates and risks reported in literature.
Updated relative risk values have been reported since the original Rising Tide report. The factors included in the analysis are presented in the table below. Hearing loss has been recently recognized as a risk factor for dementia, with studies showing that even mild levels of hearing loss increase the long-term risk of cognitive decline (Livingston, et al., 2017; Thomson, et al., 2017).
Additional factors such as education and genetics have been incorporated into the base incidence rate. By doing so, we assume that the educational profile and genetic risk profile of the population is not changing over the analysis period. Since people at risk of dementia by 2050 would already be born and have completed most of their education, the relevant genetic and educational profile of this population is not changing over time.
The ethnic groupings used in the analysis are taken from the designations used by Statistics Canada in the 2016 Population Census (Statistics Canada, 2017). When the census was completed, a long-form question asked participants to self-identify their ethnic origin and year of immigration. This information provides the basis for both the ethnic profile of the population and the primary sources of recent immigration.
While the primary countries of origin can change over time, for this analysis, it is assumed that the distribution of countries of origin and age will remain similar to that seen over the last decade. Note that while the relative rate of immigration of some ethnic groups (e.g., people of African origin) has increased compared to historical sources of immigration (e.g., Europe), the percentage of immigrants within the population evolves more slowly.
The relative risks of dementia associated with ethnicity, mapped to the Statistics Canada ethnic groupings relative to people of Asian origins, are taken from the 2016 paper by Mayada and colleagues. The risks are adjusted to account for other comorbid factors, and Mayada found no clear remaining factors to account for the differences between ethnic groups.
Historical data reconciliation
Most historical data is not available in a form that is directly usable by the agent-based model approach. For example, while the prevalence of individual conditions may be presented, the full set of comorbidities between all health states by age and sex is not available. Similarly, while the relative risk of the onset of dementia given one or two other characteristics might be found in the literature, the combined relative risk from multiple factors is often not published.
In order to combine all of the data sources into a consistent picture, a full representation of the population and all state transitions over the last 10 years is constructed such that it is aligned with all of the input data. This is not a trivial task, with billions of variables being adjusted to minimize the differences between the representation of the population and the dataset.
Once the unique profiles are consistent with the historical data, the conditional probabilities of changing from one health state to another (or for any other event such as death) can be calculated. As a validation process, the calculated transition probabilities are tested with historical data to ensure that history can be statistically reproduced. Once validated, these conditional probabilities provide the basis for the forward simulation stage.
Simulation stage
For each agent, the time of its next event is calculated using the time-dependent exponential conditional probability distributions calculated in the previous stage. Note that since the probability for most events changes with age, the probability calculation accounts for changing likelihoods over time. For the agent with the next event to occur, the state of the agent is changed (such as changing “vascular dementia” from “no” to “yes”). The time of the next event for this agent is then recalculated and the next agent is processed.
While the mechanics of the simulation stage are relatively straightforward, the underlying conditional probabilities that are used can result in complex dynamics arising within the model.
Output stage
At periodic intervals during the simulation (usually at the end of each year), the state of every agent in the system is recorded in the database, along with any changes in state that occurred since the previous output time.
Agents who have died or emigrated in the interval between outputs are no longer recorded in the output state, but their removal is recorded in the change of state. Similarly, new agents (through birth or immigration) are included in the new state output, as well as in the change of state records. This ensures that all output is internally consistent, with all agents accounted for.
Since each simulation generates stochastic output, after a set of simulations are run, statistics are calculated on the set of simulations for the variables of interest. For example, the average number of new cases of a disease for people in a given age range and geographic region can be calculated.
Dementia-specific extension
The Landmark Study model extends the basic agent to include a care partner trait, which is a link to another agent in the model. When a person has dementia, there is probability (based on age) that a person will require a care partner.
Using the family structure of the person with dementia, and the distribution of people who provide unpaid caregiving (such as partners, children, or friends), another appropriate agent in the model is identified as a care partner.
- Appendix References
-
Akbaraly, Singh-Manoux, A., Dugravot, A., Brunner, E. J., Kivimäki, M., & Sabia, S. (2019). Association of midlife diet with subsequent risk for dementia. Journal of the American Medical Association, 321(10), 957–968. https://doi.org/10.1001/jama.2019.1432
Byers, A. L., & Yaffe, K. (2011). Depression and risk of developing dementia. Nature Reviews Neurology, 7(6), 323–331. https://doi.org/10.1038/nrneurol.2011.60
Cerasuolo J. O., Cipriano, L. E., Sposato, L. A., Kapral, M. K., Fang, J., Gill, S. S., Hackam, D. G., & Hachinski, V. (2017). Population-based stroke and dementia incidence trends: Age and sex variations. Alzheimer’s & Dementia, 13(10), 1081–1088. https://doi.org/10.1016/j.jalz.2017.02.010
Feder K., Michaud, D., Ramage-Morin, P., McNamee, J., & Beauregard, Y. (2015). Prevalence of hearing loss among Canadians aged 20 to 79: Audiometric results from the 2012/2013 Canadian Health Measures Survey. Health Reports, 26(7), 18–25. https://www150.statcan.gc.ca/n1/pub/82-003-x/2015007/article/14206-eng.pdf
Gudala K., Bansal, D., Schifano, F., & Bhansali, A. (2013). Diabetes mellitus and risk of dementia: A meta-analysis of prospective observational studies. Journal of Diabetes Investigation, 4(6), 640–650. https://doi.org/10.1111/jdi.12087
Gurgel R. K., Ward, P. D., Schwartz, S., Norton, M. C., Foster, N. L., & Tschanz, J. T. (2014). Relationship of hearing loss and dementia: A prospective, population-based study. Otology & Neurotology, 35(5), 775–781. https://doi.org/10.1097/MAO.0000000000000313
Haroon, N. N., Austin, P. C., Shah, B. R., Wu, J., Gill, S. S., & Booth, G. L. (2015). Risk of dementia in seniors with newly diagnosed diabetes: A population-based study. Diabetes Care, 38(10), 1868–1875. https://doi.org/10.2337/dc15-0491
Hennessy D. A., Flanagan, W. M., Tanuseputro, P., Bennett, C., Tuna, M., Kopec, J., Wolfson, M. C., & Manuel, D. G. (2015). The population health model (POHEM): An overview of rationale, methods and applications. Population Health Metrics, 13(1), 24–24. https://doi.org/10.1186/s12963-015-0057-x
Kuźma E., Lourida, I., Moore, S. F., Levine, D. A., Ukoumunne, O. C., & Llewellyn, D. J. (2018). Stroke and dementia risk: A systematic review and meta-analysis. Alzheimer's & Dementia, 14(11), 1416–1426. https://doi.org/10.1016/j.jalz.2018.06.3061
Lin, F. R., Metter, E. J., O'Brien, R. J., Resnick, S. M., Zonderman, A. B., & Ferrucci, L. (2011). Hearing loss and incident dementia. Archives of Neurology, 68(2), 214–220. https://doi.org/10.1001/archneurol.2010.362
Livingston, G., Sommerlad, A., Orgeta, V., Costafreda, S. G., Huntley, J., Ames, D., Ballard, C., Banerjee, S., Burns, A., Cohen-Mansfield, J., Cooper, C., Fox, N., Gitlin, L. N., Howard, R., Kales, H. C., Larson, E. B., Ritchie, K., Rockwood, K., Sampson, E. L., … Mukadam, N. (2017). Dementia prevention, intervention, and care. Lancet, 390(10113), 2673–2734. https://doi.org/10.1016/S0140-6736(17)31363-6
Lourida I., Soni, M., Thompson-Coon, J., Purandare, N., Lang, I. A., Ukoumunne, O. C., & Llewellyn, D. J. (2013). Mediterranean diet, cognitive function, and dementia: A systematic review. Epidemiology, 24(4), 479–489. https://doi.org/10.1097/EDE.0b013e3182944410
Nabalamba A., & Patten, S. B. (2010). Prevalence of mental disorders in a Canadian household population with dementia. Canadian Journal of Neurological Sciences, 37(2), 186–194. https://doi.org/10.1017/S0317167100009914
Ng, J., Turek, M. & Hakim, A. (2013). Heart disease as a risk factor for dementia. Clinical Epidemiology, 5, 135–145. https://doi.org/10.2147/CLEP.S30621
Mayeda E. R., Glymour, M. M., Quesenberry, C. P., & Whitmer, R. A. (2016). Inequalities in dementia incidence between six racial and ethnic groups over 14 years. Alzheimer’s & Dementia, 12(3), 216–224. https://alz-journals.onlinelibrary.wiley.com/doi/10.1016/j. jalz.2015.12.007
Ott A., Stolk, R., van Harskamp, F., Pols, H., Hofman, A., & Breteler, M. (1999). Diabetes mellitus and the risk of dementia: The Rotterdam Study. Neurology, 53(9), 1937–1942. https://doi.org/10.1212/WNL.53.9.1937
Public Health Agency of Canada. (2021, December 15). Canadian chronic disease surveillance system. https://health-infobase.canada.ca/ccdss/data-tool/
Scarmeas N., Luchsinger, J. A., Schupf, N., Brickman, A. M., Cosentino, S., Tang, M. X., & Stern, Y. (2009). Physical activity, diet, and risk of Alzheimer disease. Journal of the American Medical Association, 302(6), 627–637. https://doi.org/10.1001/jama.2009.1144
Smolina K., Wotton, C. J., & Goldacre, M. J. (2015). Risk of dementia in patients hospitalised with type 1 and type 2 diabetes in England, 1998–2011: A retrospective national record linkage cohort study. Diabetologia, 58(5), 942–950. https://doi.org/10.1007/s00125-015-3515-x
Sofi F., Abbate, R., Gensini, G. F., & Casini, A. (2010). Accruing evidence on benefits of adherence to the Mediterranean diet on health: An updated systematic review and meta-analysis. The American Journal of Clinical Nutrition, 92(5), 1189–1196. https://doi.org/10.3945/ajcn.2010.29673
Statistics Canada. (2019, June 18). Census profile, 2016 census. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E
Tariq, & Barber, P. A. (2018). Dementia risk and prevention by targeting modifiable vascular risk factors. Journal of Neurochemistry, 144(5), 565–581. https://doi.org/10.1111/jnc.14132
Thomson, R. S., Auduong, P., Miller, A. T., & Gurgel, R. K. (2017). Hearing loss as a risk factor for dementia: A systematic review. Laryngoscope Investigative Otolaryngology, 2(2), 69–79. https://doi.org/10.1002/lio2.65
Tolppanen A., Ngandu, T., Kåreholt, I., Laatikainen, T., Rusanen, M., Soininen, H., & Kivipelto, M. (2014). Midlife and late-life body mass index and late-life dementia: Results from a prospective population-based cohort. Journal of Alzheimer’s Disease, 38(1), 201–209. https://doi.org/10.3233/JAD-130698
